Pfizer and Moderna mRNA vaccines yield a robust antibody response even when people don’t develop significant side effect symptoms following vaccination, a new study shows.
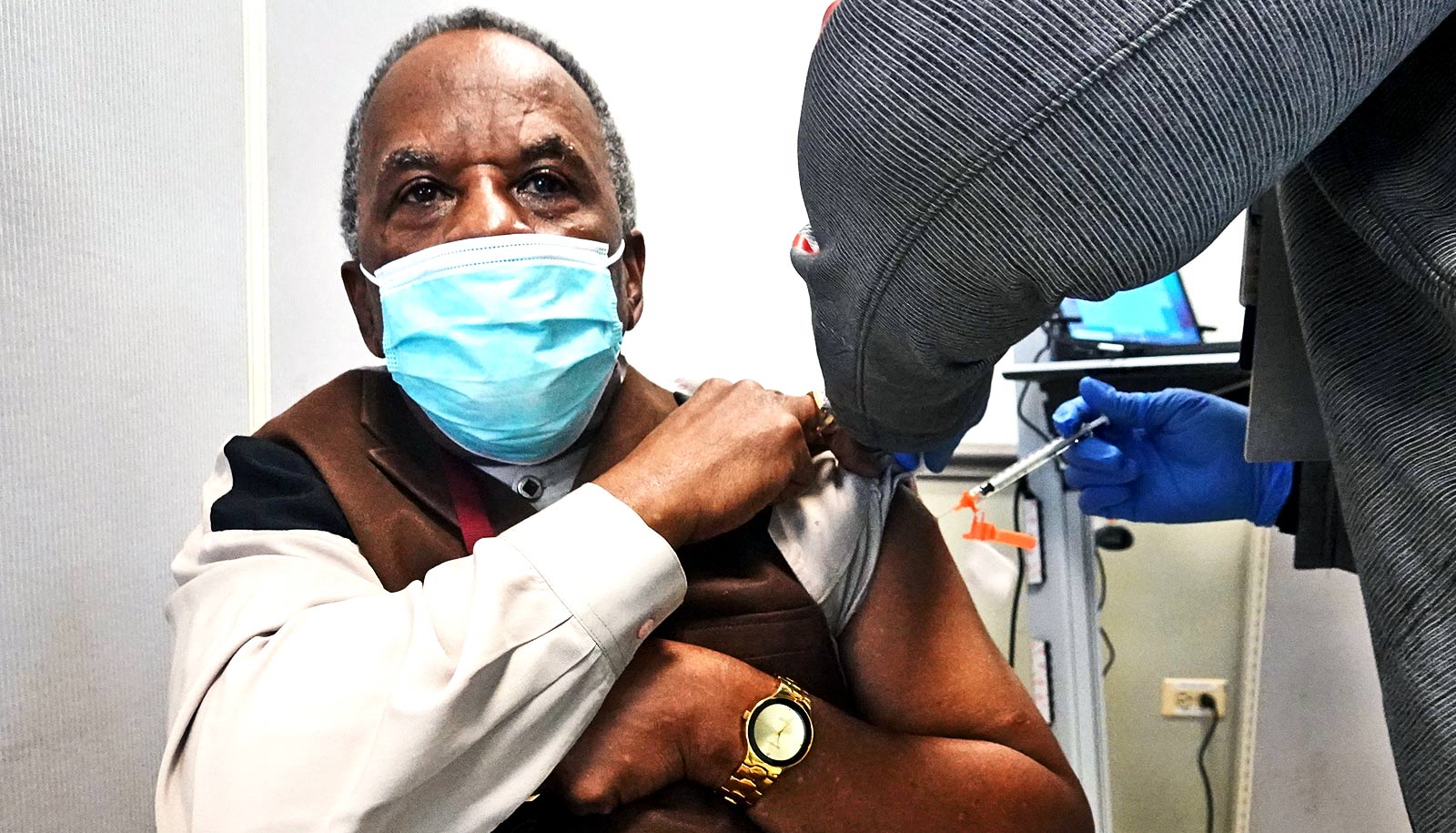
When the two messenger RNA vaccines for COVID-19 first became readily available, many people talked about side effects, everything from headaches to chills to feeling exhausted for a couple days. Yet plenty of others seemed to take the shots in stride, barely registering much beyond a sore arm.
It was popular to assume that feeling lousy was a good thing, a sign that your body was working overtime to develop its defenses against COVID.
Researchers conducted a study of nearly 1,000 health care workers in the Johns Hopkins Health System who received two doses of either the vaccine manufactured by Pfizer/BioNTech or Moderna. The findings appear in JAMA Internal Medicine.
The two mRNA vaccines evaluated in the study introduce the body’s immune system to S1, a protein subunit that’s a component of the spikes found on the surface of SARS-CoV-2. The spikes enable the virus to latch onto healthy cells and infect them.
Immunoglobulin G (IgG) antibodies elicited by S1 from the vaccines stimulating the immune system neutralize the virus particles, preventing infection by SARS-CoV-2, or at least reducing the severity of the disease.
“It wasn’t known if a lack of symptoms following vaccination or prior SARS-CoV-2 infection would indicate a less-than-adequate antibody response in people who received either the Pfizer/BioNTech or Moderna vaccines, so we studied an available group of staff from our hospital to see if there were any connections,” says senior author Aaron Milstone, associate hospital epidemiologist at Johns Hopkins Hospital.
The researchers recruited 954 Johns Hopkins Medicine health care workers who had received both doses of either the Pfizer or Moderna vaccines, including some who had a known prior SARS-CoV-2 infection. Infection was defined as having a positive SARS-CoV-2 PCR test result prior to 14 days after a second vaccine dose or a high IgG antibody count against S1 prior to vaccination.
Participants self-reported side effect symptoms following vaccination as none, mild (injection site pain, mild fatigue, or headache), or clinically significant (fatigue, fever, or chills).
Clinically significant symptoms were reported by 52 (5%) of the participants after the first vaccine dose and by 407 (43%) after the second shot. After adjusting for prior SARS-CoV-2 infection, age, and sex, the odds of clinically significant symptoms following either dose were higher among those who received the Moderna vaccine. Prior SARS-CoV-2 infection was associated with increased odds of clinically significant symptoms following one dose but not two.
Regardless of symptoms, nearly all participants (953 of 954, or 99.9%) developed spike IgG antibodies 14 or more days following the administration of the second dose. The one person who did not have IgG antibodies was taking an immunosuppressant medication.
Factors that were independently associated with higher median IgG levels (after adjusting for time following the second vaccine dose) were reporting of clinically significant symptoms, age younger than 60, being female, receipt of the Moderna vaccine, and prior SARS-CoV-2 exposure.
“The findings suggest that either spike mRNA vaccine will work well against SARS-CoV-2, even if a person doesn’t experience symptoms after vaccination or if they had a prior infection by the virus,” says lead author Amanda Debes, assistant scientist in international health at the Johns Hopkins Bloomberg School of Public Health. “This should help reduce anxieties that the vaccines will be less effective in either situation.”
Source: Johns Hopkins University