An investigational vaccine designed to protect against COVID-19 produced both binding and neutralizing antibodies in healthy adult volunteers, according to interim results of an ongoing phase 1 trial.
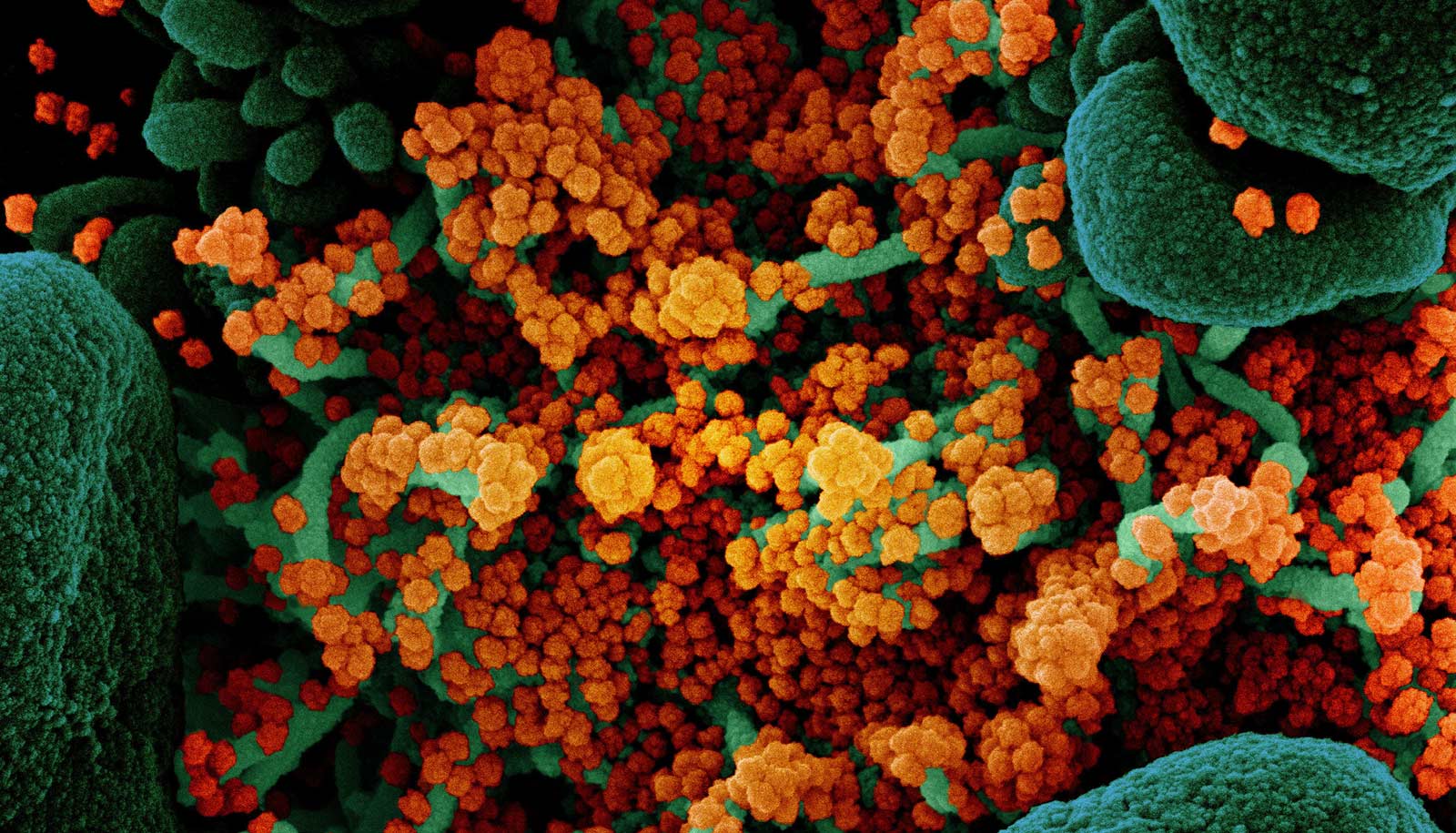
Researchers designed the experimental vaccine, mRNA-1273, to induce neutralizing antibodies directed at a portion of the coronavirus “spike” protein, which the virus uses to bind to and enter human cells.
Researchers at NIAID and at Moderna, Inc. of Cambridge, Massachusetts are developing the vaccine. Emory University’s Vaccine and Treatment Evaluation Unit (VTEU) was one of two sites in the nation that tested the vaccine.
“These interim results are very encouraging,” says principal investigator Evan Anderson, associate professor of medicine and pediatrics at Emory University School of Medicine and Children’s Healthcare of Atlanta.
“While there is still a lot of work to do before we have a vaccine that is proven to be safe and effective against COVID-19, this study provides critical information about the safety of the vaccine. Importantly, the vaccine resulted in a robust immune response.”
The interim report, which appears in the New England Journal of Medicine, details the initial results of the first 45 volunteers ages 18 to 55 years old. Emory enrolled 17 of those volunteers at the Hope Clinic or the Emory Children’s Clinic.
The interim analysis includes results of tests measuring levels of vaccine-induced neutralizing activity through day 43 after the second injection. Two doses of vaccine prompted high levels of neutralizing antibody activity that were above the average values seen in convalescent sera obtained from persons with confirmed COVID-19 disease.
The findings reported no serious adverse events. More than half of the volunteers reported fatigue, headache, chills, myalgia, and pain at the injection site, with systemic adverse events more common following the second vaccination and in those who received the highest vaccine dose.
“Rising COVID-19 infection rates throughout the country show that the need for a vaccine has only become more urgent,” says Nadine Rouphael, contact principal investigator at the Emory VTEU. Rouphael is also interim director of the Hope Clinic at the Emory Vaccine Center and associate professor of medicine (infectious diseases) at Emory University School of Medicine.
Anderson and Rouphael are coauthors of the study. Lisa A. Jackson, of Kaiser Permanente Washington Health Research Institute in Seattle, where the first volunteer received the vaccine on March 16, is the study’s trial lead. The consortium is led by co-principal investigators David S. Stephens, professor and chair of the department of medicine of Emory University, and Kathleen Neuzil of the University of Maryland School of Medicine.
“As the largest clinical trials network in the Division of Microbiology and Infectious Diseases at NIH, we are working to accelerate research that will identify a vaccine to combat COVID-19,” says Stephens. “We are excited about the promise of these early results and ready for the challenging work that lies ahead.”
A phase 2 clinical trial of mRNA-1273, sponsored by Moderna, Inc., began enrollment in late May and plans are underway to launch a phase 3 efficacy trial in July 2020.
Additional information about the trial design is available at clinicaltrials.gov using the identifier NCT04283461.
Source: Emory University