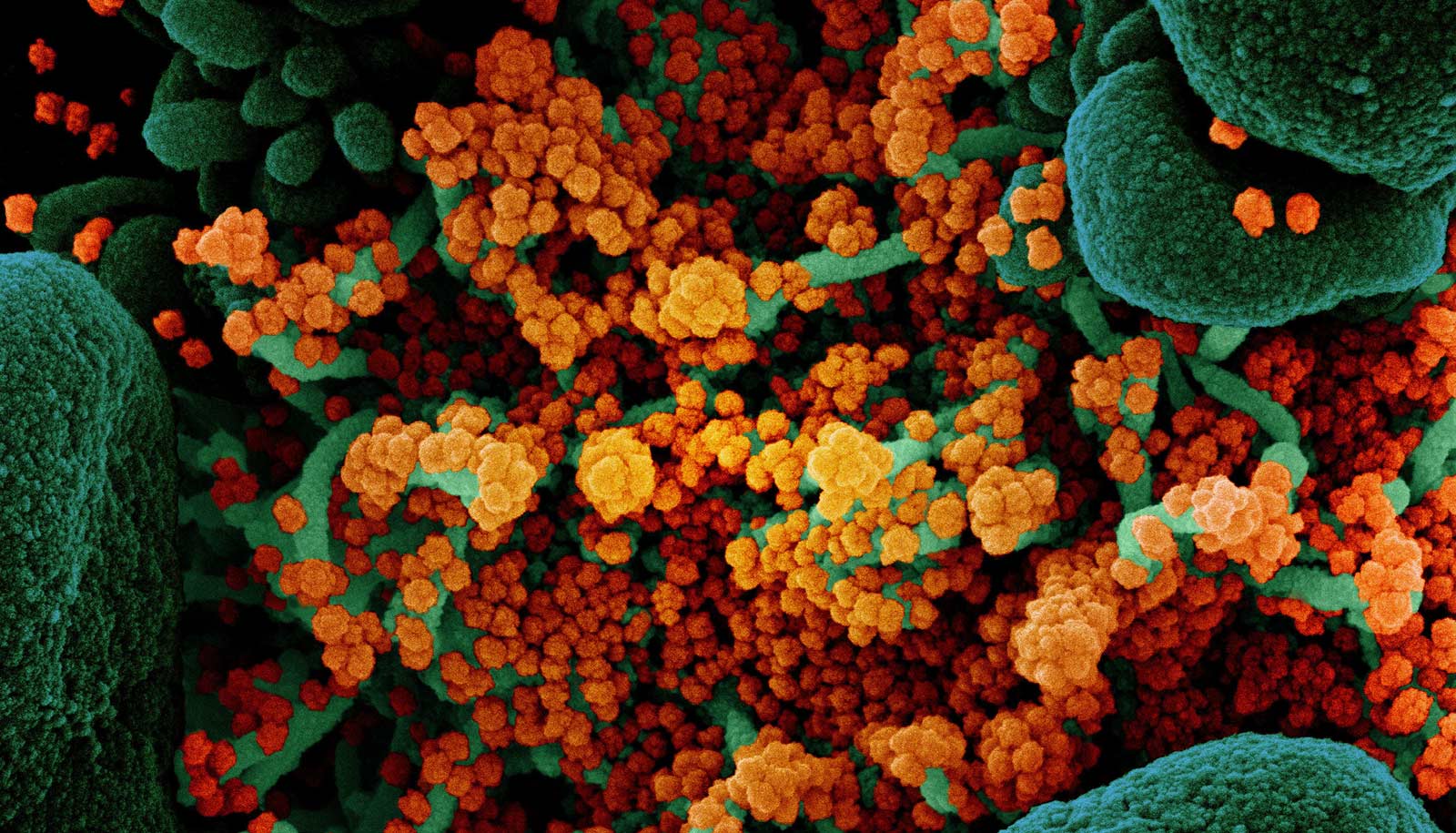
Once a COVID-19 vaccine is proven to be both safe and effective, governments, industry, and health care providers will face the considerable task of figuring out how to distribute the vaccine fairly and efficiently.
This is precisely the sort of challenge Julie Swann has spent her professional life preparing for. Swann, department head and professor of the industrial and systems engineering at North Carolina State University, uses mathematical models to make health care and supply chains more efficient, effective, and equitable.
Vaccine distribution involves health care and supply chains, as well as issues of efficiency, efficacy, and equality. In other words, the task of getting a COVID-19 vaccine to the most number of people is right up Swann’s alley.
Here, she explains more about what institutions should be doing now to prepare themselves for future challenges related to vaccine distribution:
So, there are a couple scenarios to consider, if and when COVID-19 vaccines become available. One scenario is that there is plenty of vaccine, and we have to figure out how to distribute 300 million doses efficiently. What questions or challenges does that raise?
Wow, I would love for that to be the case. If we have that much vaccine available simultaneously, then the challenge is to get administered to as many people as possible, as quickly as possible.
To make it geographically accessible, we would want to distribute broadly, including to rural locations and multiple points of distribution within urban areas. We also want to send it to places where people are likely to want vaccine. These places can include many types of healthcare providers, such as primary care physicians, specialty providers, Federally Qualified Healthcare Clinics, hospitals, and nursing homes. But you also want to think about other locations, like pharmacies, retail clinics, workplaces, prisons, military bases or schools, that can meet people where they are and at different times of the day. You also need to take into account that the vaccine needs to be affordable, and that’s for the total cost of the vaccine itself and the administration fee to obtain it. Throughout all of this, there will need to be an educational campaign that informs people on why to get a vaccine and how they can do so.
It is possible that multiple doses may be needed, so we will need good information systems to monitor who has received what and when. We also saw for H1N1, in 2009 and 2010, that leftover vaccine was considered “hazardous waste” by some states. So it is important to know where leftover vaccine is located in case it needs to be recollected and disposed.
It would also be great if we can think about how to help others worldwide who are struggling with this pandemic. If we have that much vaccine, I hope we are working with other countries to make sure they have sufficient supply, too.
Is this scenario, of there being an ample supply of vaccine all at once, even remotely likely?
We know that there are multiple companies working on solutions, and the government is investing in multiple supply chain and distribution efforts simultaneously. We certainly hope for a solution that leads to enough vaccine to cover everyone simultaneously.
Unfortunately we also know that the challenge we are undertaking is unprecedented—we have never had a vaccine for a coronavirus, and we have never produced enough product virtually overnight to cover the entire country simultaneously. It is my expectation that we will have shortages, at least in the beginning.
Okay, so the second scenario is that there will not be enough vaccine for everyone at first, meaning that vaccine will have to be distributed as it becomes available. This raises questions about how to distribute the vaccine efficiently, but it also raises some very tricky questions about fairness. What goes in to deciding how we prioritize access to COVID-19 vaccines?
Great question. There is the question of who should receive it based on exposure or risk. For that, there is a standing group of medical experts that provides scientifically guided advice related to vaccines. For H1N1, it was that group, the Advisory Committee on Immunization Practices (ACIP), which outlined the priority groups to receive the H1N1 vaccine in the US. (The World Health Organization also has such a working group.)
For H1N1, the priority groups included pregnant women, caregivers for infants, health care and emergency services personnel, children and youths up to 24 years old, and people ages 25 to 64 who have medical conditions that put them at increased risk for severe outcomes. For COVID-19, the risks are different, so I would expect the targeting to take that into account. The targeting might include people with specific medical conditions such as diabetes, people of increased ages who are at greater risk of mortality, health care workers, etc.
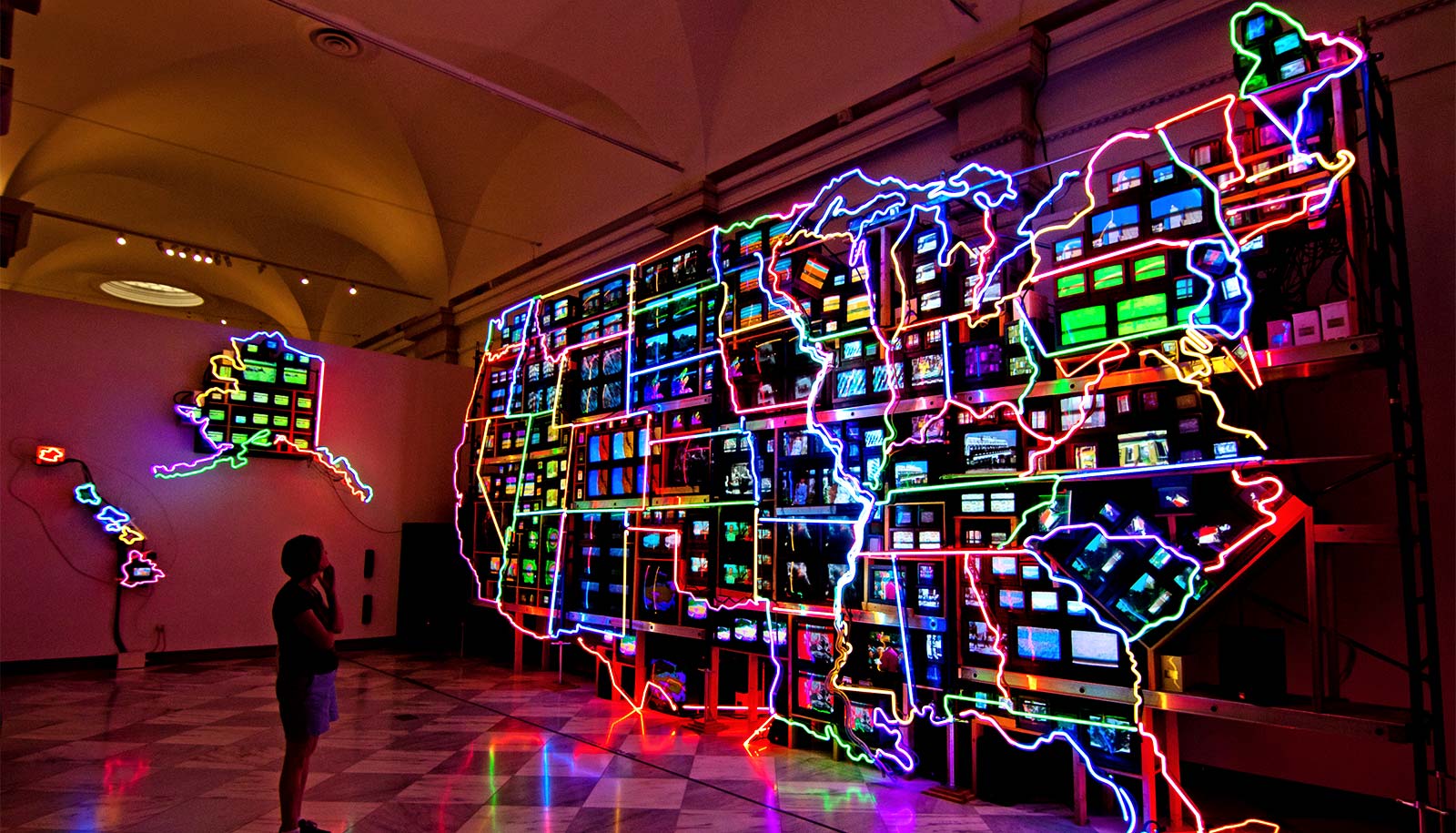
It isn’t just who needs it, though. There is also the question of fairness throughout the United States. For H1N1 a decision was made that the limited supply of vaccine would be made available “pro-rata” to each state, which means each state would receive an amount of vaccine in proportion to the size of its population. That meant that each person in the US had the same fair shot at getting a vaccine, whether they lived in New York or Wyoming. Most Americans wouldn’t want to think the vaccine is being distributed according to income, for example, or based on who represents them in Congress, or preferentially for some employers. There needs to be a transparent allocation that is well understood.
Given that equitable distribution of vaccines is, at least in part, a question of ethics, how can computer models help us arrive at a solution?
It’s an interesting intersection, isn’t it? We can think of problems in terms of our objectives, which in this case might include efficiency (speed), effectiveness (avert deaths), and equity across the population. In public health, equity can be defined in different ways, including geographically (urban and rural) or by population (pro-rata). It can also be defined in terms of outcomes. For example, right now we know that communities of color, including African Americans, Hispanics, and Native Americans, are experiencing much higher rates of COVID-19 mortality than whites, and we know that people who are older or have high-risk medical conditions are also experiencing greater mortality than others.
Computer models can do many things to help with equitable distribution of vaccines. One really important role is to project the impact of different vaccination scenarios or strategies. For example, if there are limited vaccines, what is the impact of vaccinating essential workers, or ones who might interact with a vulnerable group (e.g., nursing home workers)? If there is a group at lower direct risk (e.g., children) who have significant contact with people at risk (parents or grandparents), what would be the impact of vaccinating them? If a vaccine requires two doses, or if immunity wanes after a time period, what strategies can avert the most hospitalizations and deaths? Which strategies would be most effective at reducing the disparities in COVID-19 outcomes associated with communities of color? These are just a few examples of many different decisions where humans could be aided by input from computer models.
Your work has examined many of the variables that can affect the distribution of vaccines. For example, you have an entire paper that focuses specifically on the value of inventory information in allocating a limited supply of flu vaccine during a pandemic. Is inventory information really a challenge? Does vaccine just get lost in transit or what? Am I just not understanding what vaccine inventory means here?
Haha, good point. The question here is whether the organization who is allocating vaccine knows where the final dose is located at a particular time. Surprisingly, the answer was no during the H1N1 campaign response. States were allocated an amount of vaccine, each state decided the process to use for ordering, and shipments were made from several distribution centers. Those shipments could go to a centralized warehouse, or to a provider, who might choose to distribute it to additional locations. States were required to report the number of vaccines administered (e.g., how many given to pregnant women, or children, etc.). However, most states did not really know who had how much vaccine left at any given time. This also caused problems at the end of the campaign, when it was realized that leftover vaccine was considered as hazardous waste by some states and had to be recollected.
The system for vaccine is much like the system for distributing Coca-Cola products. The Coca-Cola Company (TCC) doesn’t necessarily know how many bottles are sitting in a particular convenience store, or when a product is purchased by a consumer, or when a location is out of stock. If the information system and collaborations have been put in place, then they know through data sharing. For example, Walmart or Publix may share information back with TCC, who can then use the information to make decisions on production, distribution, allocation, promotional campaigns, etc.
States should be investing now in information systems that can show where vaccine is, who has been vaccinated, and how much vaccine is left. This is especially important given the fact that this is a vaccine for a new class of viruses, and we will want to be tracking safety carefully. Many states may choose to use their existing vaccine information registries, so it may be a matter of adding some functionality to that system if they have not already updated their systems since the H1N1 response.
So, how do you allocate vaccine if you don’t have good inventory data? And what difference does it make if you can account for vaccine inventory and where things are in the supply chain?
For H1N1, a lot of the decisions were made based on requests from providers. Providers, in turn, were estimating how many patients they would serve. Sometimes they got it right, and sometimes they didn’t, or things changed. There were certainly time periods during H1N1 when some locations were out of stock of a vaccine while others in a different location or category of provider might have had vaccine doses available.
If you know where your inventory is, then you can inform people who want it how to get it. (It’s like those billboards at the airport telling you how many parking spots are available on a particular floor.) If you know where your inventory should be but isn’t, then you know where to send the next batch of products to meet demand. You can even do so in a way that is fair and transparent. For example, you can only send products to places who used up the products that they already received. You can also use the information on places with insufficient demand to create targeted educational approaches to increase uptake of vaccine in a particular area. For example, targeting areas that have a high rate of diabetes.
As is the case with Coca-Cola, I can tell you that a system is a lot more effective if the company that makes the products and distributes them knows when and where they are sold. The same is true of the public health system.
You’ve also done work looking at systemic factors that contribute to higher vaccination rates. What did you learn there?
We looked at the ways that different states organized their distribution systems, recognizing that there was a very short window to make those decisions in 2009 and that a campaign of that type had never been run before.
During the main time of the shortage, we found that the faster a state was able to get items shipped to providers, the more people got vaccinated. The shipment process was partly a function of how the state took orders and allocated products to providers, which is part of the supply chain design. For targeted populations, we found that higher vaccination was associated with particular types of providers, such as schools for vaccinating children. Interestingly, we found that for high-risk adults, coverage was higher with shipments to pharmacy and retail locations (not necessarily specialty providers).
We found generally that coverage for the H1N1 vaccine was also associated with other aspects of the public health system. For example, states that had higher seasonal influenza vaccine rates or more women receiving a Pap smear also had higher coverage rates. This could suggest continuing to invest in public health programs, educational campaigns, etc., to generally raise the utilization of preventive services.
Many states are struggling with trying to deal with the ongoing outbreak. However, it is also important to be thinking now about how to design the distribution system for the COVID-19 vaccines, so that we can deliver them quickly to the maximum number of people.
There is currently a great deal of uncertainty about COVID-19 vaccines, including when they might become available, whether people will need multiple doses over time, and so on. Given that uncertainty, what can or should federal, state, and local policymakers be doing to prepare for the day when vaccines will become available?
We cannot wait until vaccine is available to begin designing our systems for distributing the vaccine. We should plan for several different scenarios, including ones where vaccine is in short supply and ones where vaccine is readily available. We need to think about what these systems would look like if multiple doses are needed, and what investments we need to make in our information systems now. We can also build partnerships between public health and private industry, such as occurred with retail pharmacies. These partnerships could also help inform best practices on information in the vaccine system, just as we have for beverages or other products that we consume.
How should authorities prioritize those efforts?
That’s a difficult question. We need to do it all, and do it all right now. That is, we need to continue monitoring COVID-19, putting in place interventions to mitigate disease spread, while thinking about the future of when a vaccine will be available. The topic of vaccine distribution would be a great one on which to engage with people in universities and companies, who do a lot of thinking about supply chains. The public health perspective is also critical, because “fairness” is just one example of something that can be important when distributing vaccines (as compared to distributing beverages). Academics in particular like to think about the future and how we can best get there, so we would love to partner with federal, state, and local entities on this.
Source: NC State