A new study suggests the mortality rate from COVID-19 may be lower than previous reports have indicated.
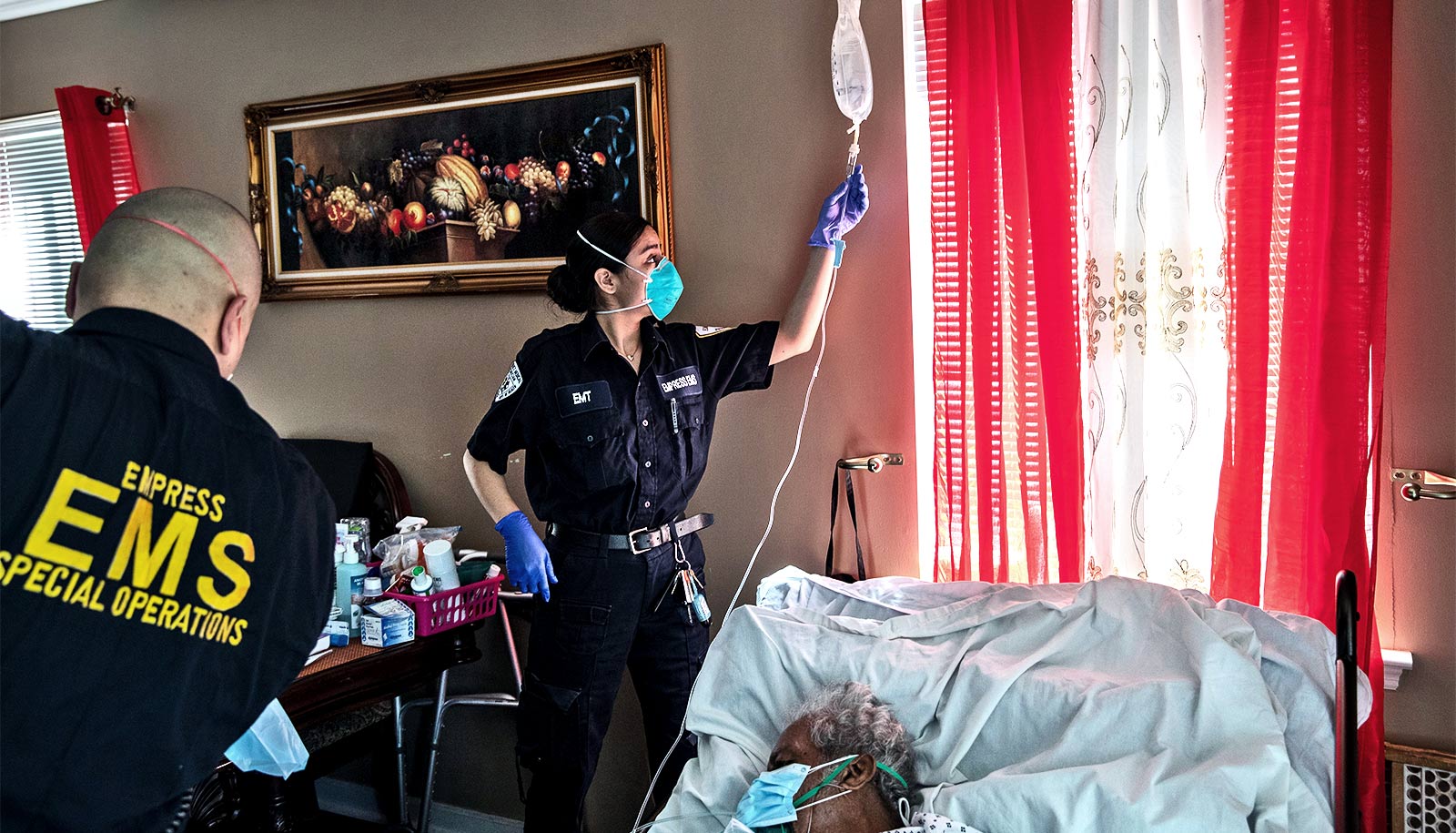
As COVID-19 has become the leading cause of death in the US, researchers at Emory University report a lower number of deaths than what most have reported for critically ill COVID-19 patients using mechanical ventilation. The research and outcomes appear in the journal Critical Care Medicine.
The researchers conducted a review of critically ill adult patients diagnosed with COVID-19, the disease caused by the coronavirus, SARS-CoV-2, across its academic health system. From March 6 through April 17, 2020, 217 critically ill adults with COVID-19 infection were admitted to six COVID-designated intensive care units (ICUs) at three Emory Healthcare acute-care hospitals.
In contrast to previous reports from Wuhan, China, Italy, and Seattle, where mortality rates ranged from 50 to 97%, Emory researchers reported a mortality rate of 35.7% for patients who required mechanical ventilation (59 patients died out of 165 who received mechanical ventilation) and an overall mortality rate of 30.9% (67 patients died out of 217 in the study) to date. Of that overall number, 60.4% of patients (131 patients out of 217 in the study) have survived to hospital discharge.
“While any death related to COVID-19 is tragic, we felt it was important to share these outcomes among COVID-19 patients requiring ICU admission and mechanical ventilation,” says Sara Auld, assistant professor in the Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine and first author of the paper.
“Other reports, both in the US and globally, have painted a starkly different picture with mortality rates often exceeding 50% in ventilated, critically ill COVID-19 patients. Our early experience indicates that the majority of patients can survive their critical illness.”
About the patients in the study
Among the 217 patients in the study population, 147 (67.7%) have been transferred alive from the ICU, 62 patients (28.6%) died in the ICU (five additional deaths occurred among patients transferred to the floor), and eight (3.7%) remained in the ICU as of May 7.
“In contrast to some of the earliest reports on mortality in COVID-19 ventilated patients, our data provide evidence that COVID-19 mortality rates can be comparable to those seen with ARDS (acute respiratory distress syndrome) due to other causes,” says David J. Murphy, associate professor in the Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine and senior author of the paper.
“These findings suggest that clinical outcomes and survival from the virus may be better than initially reported.”
In the study, the median patient age was 64, with 49 patients who were 75 years or older. Of 217 patients in the study, 98 were women, and the majority of patients (70.5%) were African American. Hypertension, or high blood pressure, was the most common additional health condition in this population of patients (134 patients) followed by diabetes (99 patients). Twenty-one patients were morbidly obese.
“There has been growing concern among both the public and the medical community that survival among those requiring mechanical ventilation was particularly low,” says Mark Caridi-Scheible, assistant professor in the department of anesthesiology in the Division of Critical Care Medicine and co-first author of the paper. “Our hope is that these data can provide some reassurance to medical providers and communities that mechanical ventilation continues to be a life-saving intervention.”
In the study, mortality was associated with older age, with 42.5% mortality in those ages 65 and above as compared to 11.3% in those under age 55. Mortality was also associated with the presence of coronary artery disease, severity of illness on arrival to the ICU, and the need for interventions including mechanical ventilation and dialysis.
“Race and sex did not differ in terms of survival, but patients who died were less likely to be morbidly obese and more likely to have underlying renal disease,” says Caridi-Scheible.
Why the different outcomes?
The researchers say intense planning, the skill of care teams, and a later arrival of COVID-19 illness in Georgia likely influenced outcomes.
“While we did repurpose several existing specialty ICUs to COVID-ICUs, all critically ill patients were cared for by critical care teams with experience managing acute respiratory failure and at standard patient-to-provider and patient-to-nurse ratios,” says study coauthor Craig Coopersmith, professor of surgery and director of the Emory Critical Care Center.
“With our findings of a mortality rate of 30.9% overall and 35.7% for COVID-19 patients who received mechanical ventilation, these results suggest that many patients with acute respiratory failure from COVID-19 can recover, even for those with severe disease requiring intubation and mechanical ventilation,” says Auld.
Funding for this research came from NIH/NIAID and NIH/CTSA grants.
Source: Emory University