Inflammation from an out-of-control immune response doesn’t appear to be the main problem for the vast majority of hospitalized COVID-19 patients, a new study shows.
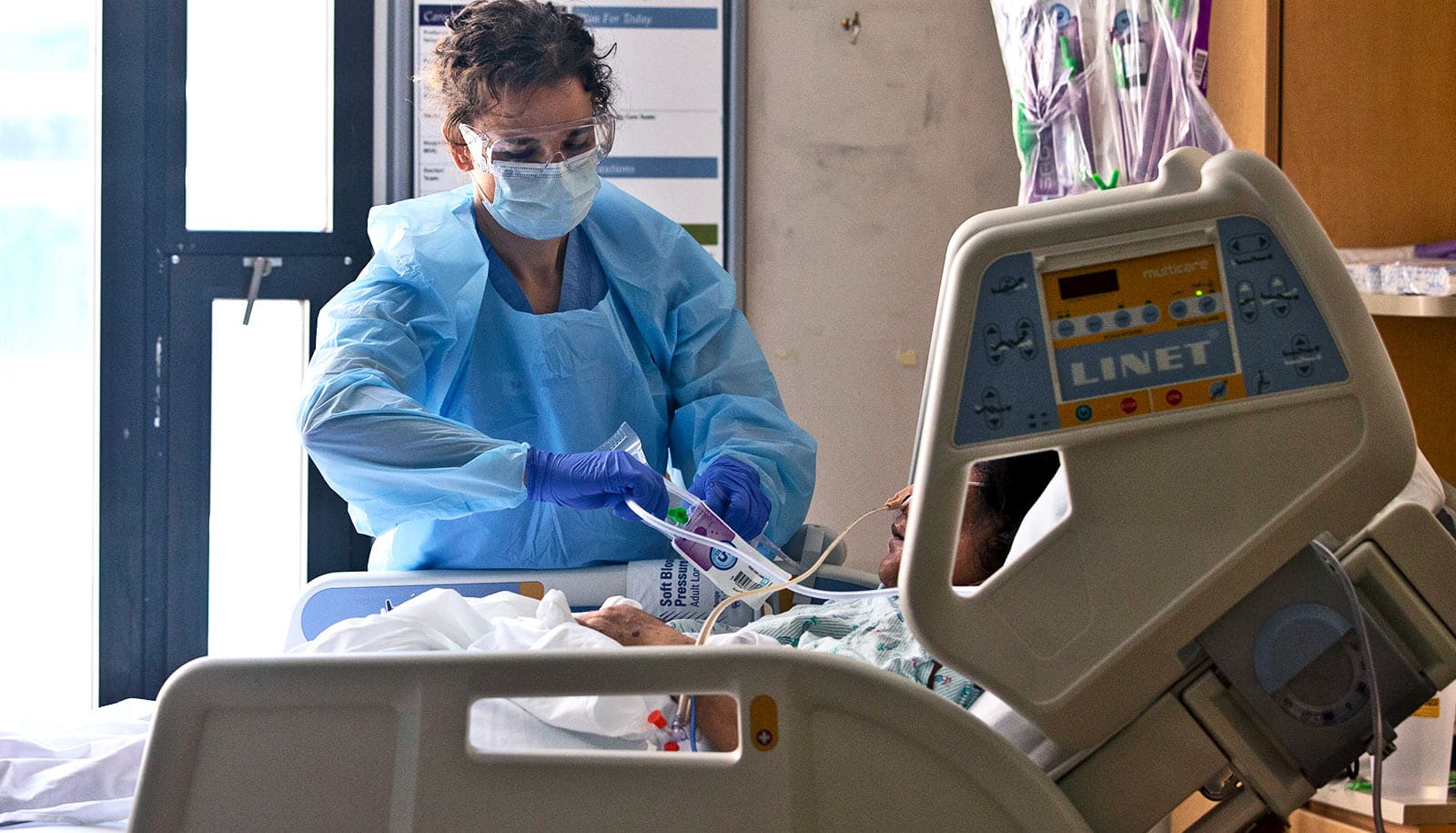
The turning point for people with COVID-19 typically comes in the second week of symptoms. As most people begin to recover, a few others find it increasingly difficult to breathe and wind up in the hospital. One theory is that those whose lungs begin to fail are victims of their own overactive immune systems.
“…lots of unproven anti-inflammatory treatments are being given to critically ill COVID-19 patients in an attempt to suppress the cytokine storm. That worries me…”
But the new study found that only 4% of patients had the sky-high levels of immune molecules that signify a so-called “cytokine storm.” The rest had inflammation, but not a remarkably high amount for people fighting infection. If anything, the COVID-19 patients had less inflammation than a comparable group of influenza patients.
The findings in Science Advances help explain why anti-inflammatory medications such as dexamethasone benefit only a fraction of people with severe COVID-19, and suggest that more research is needed to identify the causes of respiratory failure in COVID-19 patients.
“One of the very first papers published on COVID-19 patients in China reported high levels of cytokines in people in intensive care, what we might call a cytokine storm,” says co-senior author Philip Mudd, assistant professor of emergency medicine at Washington University in St. Louis, who sees patients at Barnes-Jewish Hospital.
“We wanted to have a better idea of what this cytokine storm looked like, so we began looking for it in our patients, and we were very surprised when we didn’t find it. We found that cytokine storm does happen, but it’s relatively rare, even in the COVID-19 patients that go on to have respiratory failure and require a ventilator.
“But now this idea has gotten established that respiratory failure in COVID-19 is driven by cytokine storm, and lots of unproven anti-inflammatory treatments are being given to critically ill COVID-19 patients in an attempt to suppress the cytokine storm. That worries me because such treatments are unlikely to help most people with COVID-19.”
Flu vs. COVID-19 inflammation
Before the pandemic, Mudd started investigating the immune response to influenza infection, using blood samples obtained, with consent, from flu patients who seek care in the Barnes-Jewish Hospital emergency department.
In late March, as COVID-19 patients began filling the emergency department, Mudd and co-senior author Ali Ellebedy, assistant professor of pathology and immunology and a fellow influenza expert, realized they could use the same approach to investigate how the immune response goes awry in severe cases of COVID-19.
The researchers analyzed immune cells and molecules in blood samples from 168 COVID-19 patients, 26 influenza patients, and 16 healthy people. They drew samples from influenza patients in 2019 or 2020, and from COVID-19 patients and healthy controls this year. They also collected information about how each patient fared—whether a patient ended up needing intensive care or mechanical ventilation—and whether he or she survived.
The numbers of inflammatory cells in the blood of COVID-19 and influenza patients were about the same. Seven of the COVID-19 patients (4%) showed signs of a cytokine storm, with extremely high levels of cytokines even when compared to other severely ill patients. The majority of the COVID-19 patients with acute respiratory failure not only did not have a cytokine storm, they had less inflammation than influenza patients who were equally ill.
‘Cytokine storm’ risk
A few clinical trials have shown that some severely ill COVID-19 patients improve on steroid drugs such as dexamethasone that suppress inflammation. A meta-analysis published in September placed the percentage who benefit between 2% and 9%. Those results jibe with the findings of this study, Mudd says.
“It could be that the 4% of people who have cytokine storm are the ones who benefit from steroids in those clinical trials,” Mudd says. “I think our work helps explain why steroids help some people. But from our data, it doesn’t look like most COVID-19 patients have a deficiency of steroids. If you’re giving steroids to someone who already has a lot of steroids in their body, that might not be good for them.”
The key will be to find a way to identify the people at high risk for a cytokine storm when they first arrive at the hospital, so that steroid treatment can be appropriately targeted to the ones most likely to benefit and least likely to be harmed.
“Severe flu is more inflammatory than severe COVID-19. So what’s causing their lungs to fail? We still don’t know. We’re trying to find out.”
The researchers ran a panel of routine lab tests—blood cell counts, measurements of common inflammatory markers—but could not find a signature of an impending cytokine storm. They are pursuing more in-depth analyses to find a way to predict who will develop a cytokine storm.
“The subjects in the cohort with the ‘true’ cytokine storm phenotype are such outliers immunologically compared to the others, it seems likely that there are significant differences in multiple immune pathways driving this phenotype,” Thomas says. “If we can identify features of those pathways that can be assessed quickly in a clinical setting, it could be useful for patient stratification.”
With cytokine storm largely ruled out, the cause of most cases of respiratory failure in COVID-19 patients remains unknown, Mudd says.
“In the population we studied, 24% died but only 4% had a cytokine storm,” Mudd says. “Most people who died of COVID-19 died without a cytokine storm. Severe flu is more inflammatory than severe COVID-19. So what’s causing their lungs to fail? We still don’t know. We’re trying to find out.”
Additional coauthors are from St. Jude Children’s Research Hospital and Washington University School of Medicine.
The Foundation for Barnes-Jewish Hospital, the National Institute of Allergy and Infectious Diseases of the National Institutes of Health, the Collaborative Influenza Vaccine Innovation Centers, the National Institute of Allergy and Infectious Diseases Centers of Excellence for Influenza Research and Surveillance, the St. Jude Center of Excellence for Influenza Research and Surveillance, the American Lebanese Syrian Associated Charities, and the National Center for Advancing Translational Sciences funded the work.