Researchers have discovered a method the coronavirus uses to manipulate human cells to ensure its own replication.
This knowledge will help develop drugs and vaccines to fight the coronavirus.
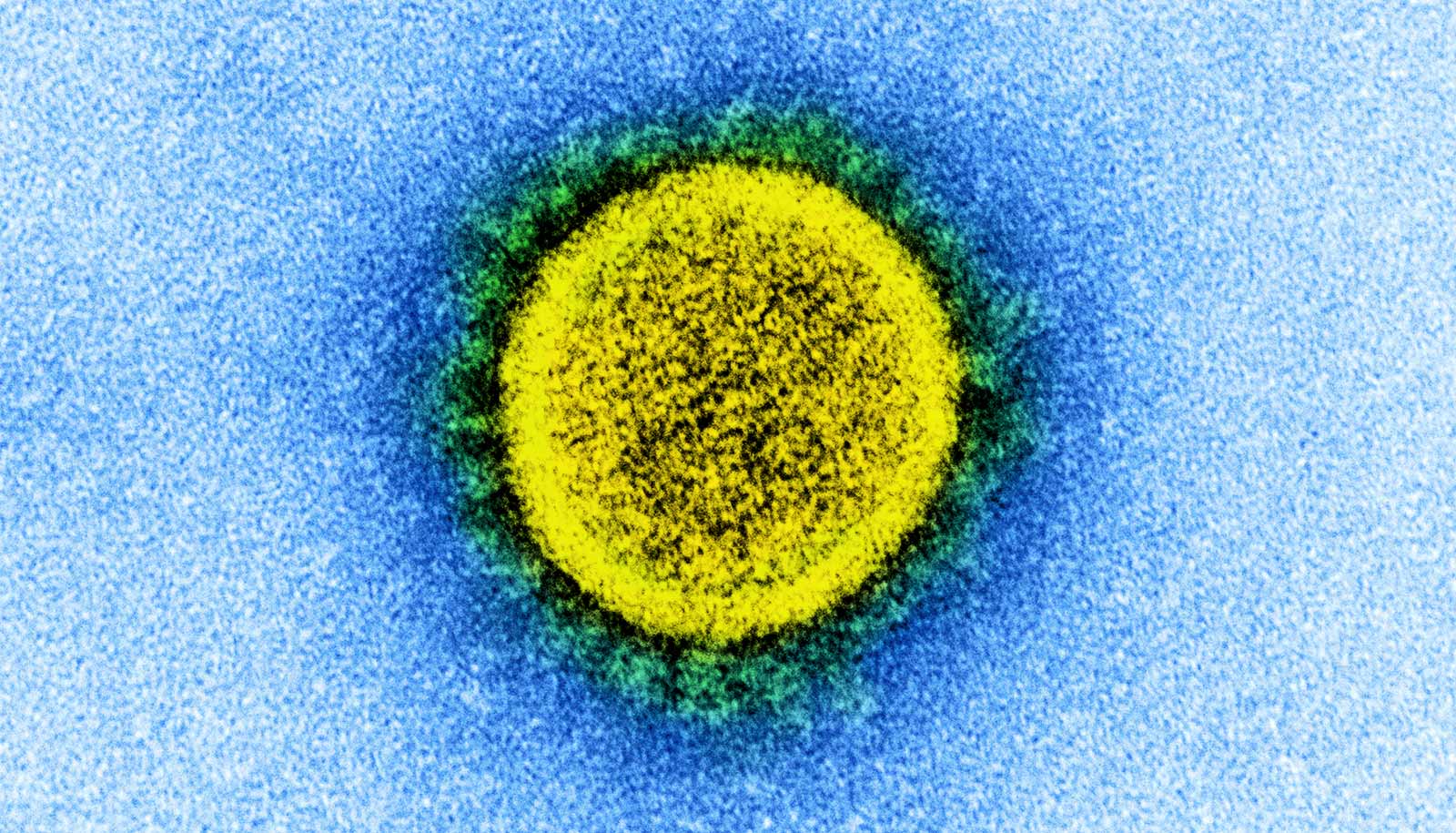
A virus takes control of an infected cell because every virus depends on the resources and molecular machines of the cell to multiply. This also applies to SARS-CoV-2, the virus that has caused the COVID-19 pandemic.
In a new study, researchers discovered a mechanism the coronavirus uses to favor the production of its proteins over infected cells’ own. The mechanism leads to cells greatly reducing the production of their own proteins, instead producing almost only viral proteins.
This not only boosts the production of new viruses, but also inhibits the immune response against the coronavirus infection.
After the virus has entered a human cell during a SARS-CoV-2 infection, the viral protein NSP1 is produced as one of the first viral proteins. Researchers already knew from other coronaviruses that NSP1 inhibits the production of the infected cell’s own proteins, but it wasn’t yet clear how this occurs.
The new work clarifies how NSP1 inhibits cellular protein production.
Ribosomes are the cellular machines that produce proteins. They read the blueprint, the messenger RNA, for a given protein and assemble the amino acids in the corresponding order. During reading, the messenger RNA passes through a channel on the ribosome.
The researchers found that NSP1 binds to this channel and blocks the ribosome. Using cryo-electron microscopy, they found they could see the binding site of NSP1 in the ribosome channel at atomic resolution.
“This detailed image provides important information for potential design of a drug that can prevent NSP1 binding without interfering with ribosomal function. If NSP1 can no longer interact with the ribosome, this allows activation of cellular defense systems that can stop viral replication,” explains coauthor Nenad Ban, professor for molecular biology at ETH Zurich.
Using biochemical and cellular experiments, the researchers were able to show that NSP1 alone is sufficient to inhibit protein production. Based on the detailed picture of the binding mode of NSP1, the researchers were able to produce modified NSP1 variants that have lost their inhibitory effect.
SARS-CoV-2 viruses with these inactive variants of the NSP1 protein will likely be attenuated, meaning they can no longer cause severe disease. Attenuated viruses can potentially be used as a vaccine. Many other vaccinations against viral diseases are already based on this principle.
The researchers were also interested in the question of why the viral proteins are produced in large quantities despite the inhibition of ribosomal function by NSP1. They found out that the viral RNA has unique properties because of which it is read very efficiently by ribosomes compared to cellular messenger RNAs.
“By NSP1 blocking ribosomes, functional ribosomes become scarce and at the same time viral RNA can make up almost half of the total RNA in the cell. Under these conditions, the viral RNA is preferentially read from the still functional ribosomes compared to the cell’s own messenger RNA,” explains coauthor Oliver Mühlemann, professor of biochemistry at the University of Bern.
The researcchers will continue to work to gain further insights into how SARS-CoV-2 manipulates the cell in its favor.
All three participating research groups are part of the National Center of Competence in Research (NCCR) RNA & Disease, which the Swiss National Science Foundation as well as the University of Bern and ETH Zurich fund. The research appears in Nature Structural & Molecular Biology.
Source: ETH Zurich