The coronavirus behind the global COVID-19 pandemic evolved from nature and not a lab, according to a new genetic study.
Researchers analyzed the genome sequence of the novel SARS-CoV-2 coronavirus that emerged in the city of Wuhan, China, last year and found no evidence that a lab or some other type of engineering made the virus.
“We determined that SARS-CoV-2 originated through natural processes by comparing the genetic sequences and protein structures of other coronaviruses to those of new virus that causes COVID-19,” says Robert F. Garry, professor of microbiology and immunology at Tulane University School of Medicine and senior author of the paper in Nature Medicine.
“It is very close to a bat virus. The adaptations that the virus has made to affect humans are actually very different than what you would expect if you were designing it using computational models in biological engineering.
Coronavirus timeline
Coronaviruses are a large family of viruses that can cause illnesses ranging widely in severity. The first known severe illness a coronavirus caused emerged with the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak in China. A second outbreak of severe illness began in 2012 in Saudi Arabia with the Middle East Respiratory Syndrome (MERS).
Last year, Chinese authorities alerted the World Health Organization of an outbreak of a novel strain of coronavirus causing severe illness, subsequently named SARS-CoV-2. As of March 17, 2020, over 179,000 cases of COVID-19 have been documented, although many more mild cases have likely gone undiagnosed. The virus has killed over 7,400 people.
Shortly after the outbreak began, Chinese scientists sequenced the genome of the novel coronavirus and made the data available to researchers worldwide. The resulting data show that the epidemic has expanded because of human-to-human transmission after an initial introduction into the human population.
The ‘backbone’ of the new coronavirus
Researchers used this sequencing data to explore the origins and evolution of SARS-CoV-2 by focusing in on several telltale features of the virus.
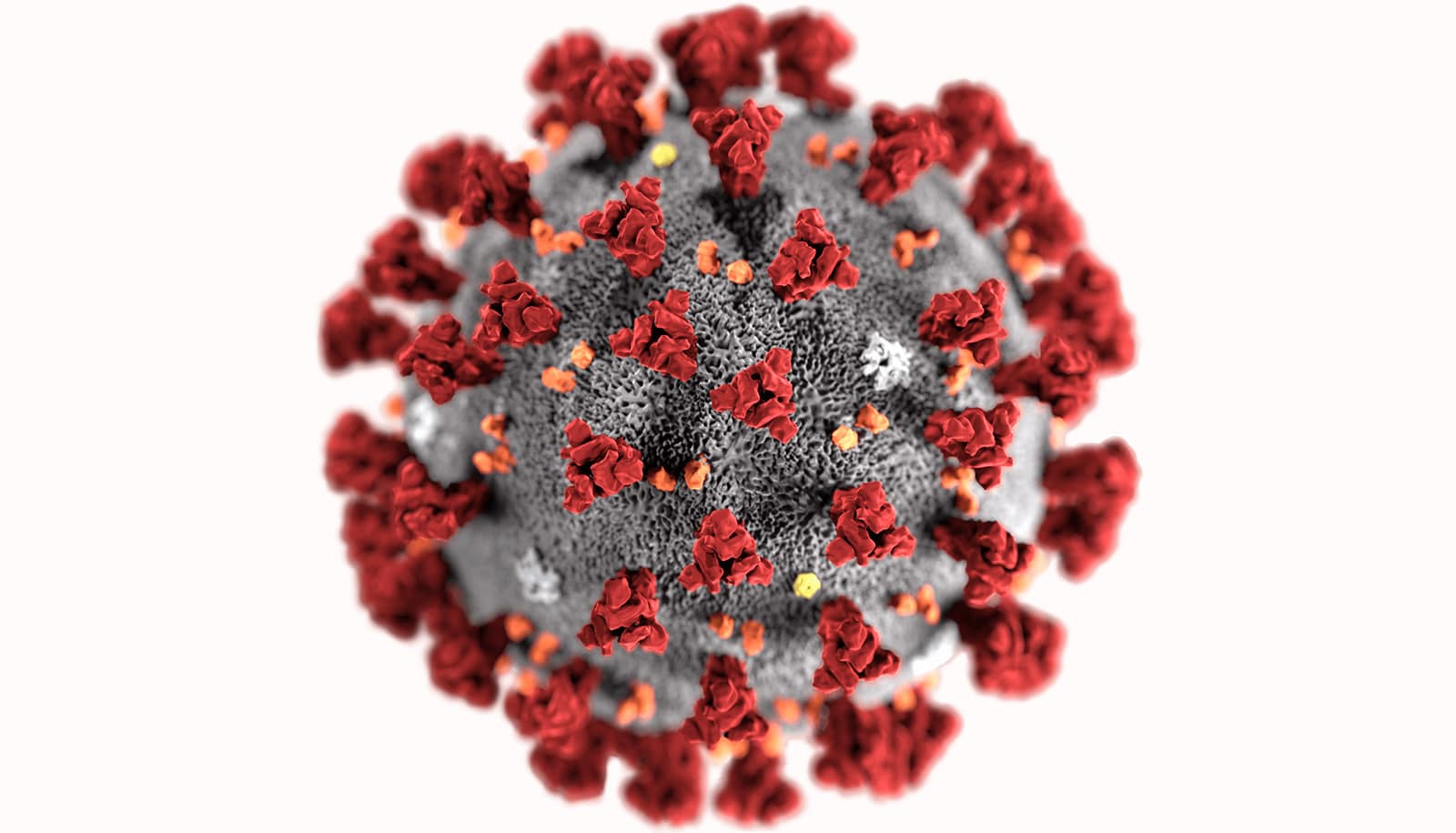
They analyzed the genetic template for spike proteins, armatures on the outside of the virus that it uses to grab and penetrate the outer walls of human and animal cells.
More specifically, they focused on two important features of the spike protein: the receptor-binding domain (RBD), a kind of grappling hook that grips onto host cells, and the cleavage site, a molecular can opener that allows the virus to crack open and enter host cells.
The scientists found that the RBD portion of the SARS-CoV-2 spike proteins evolved to effectively target a molecular feature on the outside of human cells called ACE2, a receptor involved in regulating blood pressure. The SARS-CoV-2 spike protein was so effective at binding the human cells that the scientists concluded it was the result of natural selection and not the product of genetic engineering.
Data on SARS-CoV-2’s backbone—its overall molecular structure—support this evidence for natural evolution, researchers say.
If someone wanted to engineer a new coronavirus as a pathogen, they would have constructed it from the backbone of a virus known to cause illness. But the scientists found that the SARS-CoV-2 backbone differed substantially from those of already known coronaviruses and mostly resembled related viruses found in bats and pangolins.
“These two features of the virus, the mutations in the RBD portion of the spike protein and its distinct backbone, rules out genetic engineering as a potential origin for SARS-CoV-2” says coauthor Kristian Andersen, an associate professor of immunology and microbiology at Scripps Research.
The first of two scenarios
Based on their genomic sequencing analysis, Garry and his colleagues conclude that the most likely origins for SARS-CoV-2 followed one of two possible scenarios.
In one scenario, the virus evolved to its current pathogenic state through natural selection in a non-human host and then jumped to humans—how previous coronavirus outbreaks have emerged, with humans contracting the virus after direct exposure to civets (SARS) and camels (MERS).
The researchers proposed bats as the most likely reservoir for SARS-CoV-2 as it is very similar to a bat coronavirus. There are no documented cases of direct bat-human transmission, however, suggesting that an intermediate host likely occurred between bats and humans.
In this scenario, both of the distinctive features of SARS-CoV-2’s spike protein—the RBD portion that binds to cells and the cleavage site that opens the virus up—would have evolved to their current state prior to entering humans. In this case, the current epidemic would probably have emerged rapidly as soon as humans became infected, as the virus would have already evolved the features that make it pathogenic and able to spread between people.
And the second
In the second proposed scenario, a non-pathogenic version of the virus jumped from an animal host into humans and then evolved to its current pathogenic state within the human population. For instance, some coronaviruses from pangolins, anteater-like mammals found in Asia and Africa, have an RBD structure similar to that of SARS-CoV-2.
A coronavirus from a pangolin could possibly have been transmitted to a human, either directly or through an intermediary host such as civets or ferrets. Then the other distinct spike protein characteristic of SARS-CoV-2, the cleavage site, could have evolved within a human host, possibly via limited undetected circulation in the human population prior to the beginning of the epidemic.
The researchers found that the SARS-CoV-2 cleavage site, appears similar to the cleave sites of strains of bird flu that has been shown to transmit easily between people. SARS-CoV-2 could have evolved such a virulent cleavage site in human cells and soon kicked off the current outbreak, as the coronavirus would possibly have become far more capable of spreading between people.
“It is pretty well-adapted to humans. That’s one of the puzzles we’re trying to understand as we examine the virus. It could have been circulating in humans for a while now,” Garry says.
Additional coauthors are from Columbia University, the University of Sydney, and the University of Edinburgh. The National Institutes of Health and the Pew Charitable Trusts funded the work.
Source: Tulane University