Researchers have redesigned an enzyme proven to help regrow damaged nerve tissue in animals but too unstable for use in humans, researchers report.
With stability added, researchers could potentially repurpose the enzyme, chondroitinase ABC, to help reverse the nerve damage strokes cause and as a treatment for spinal cord injuries.
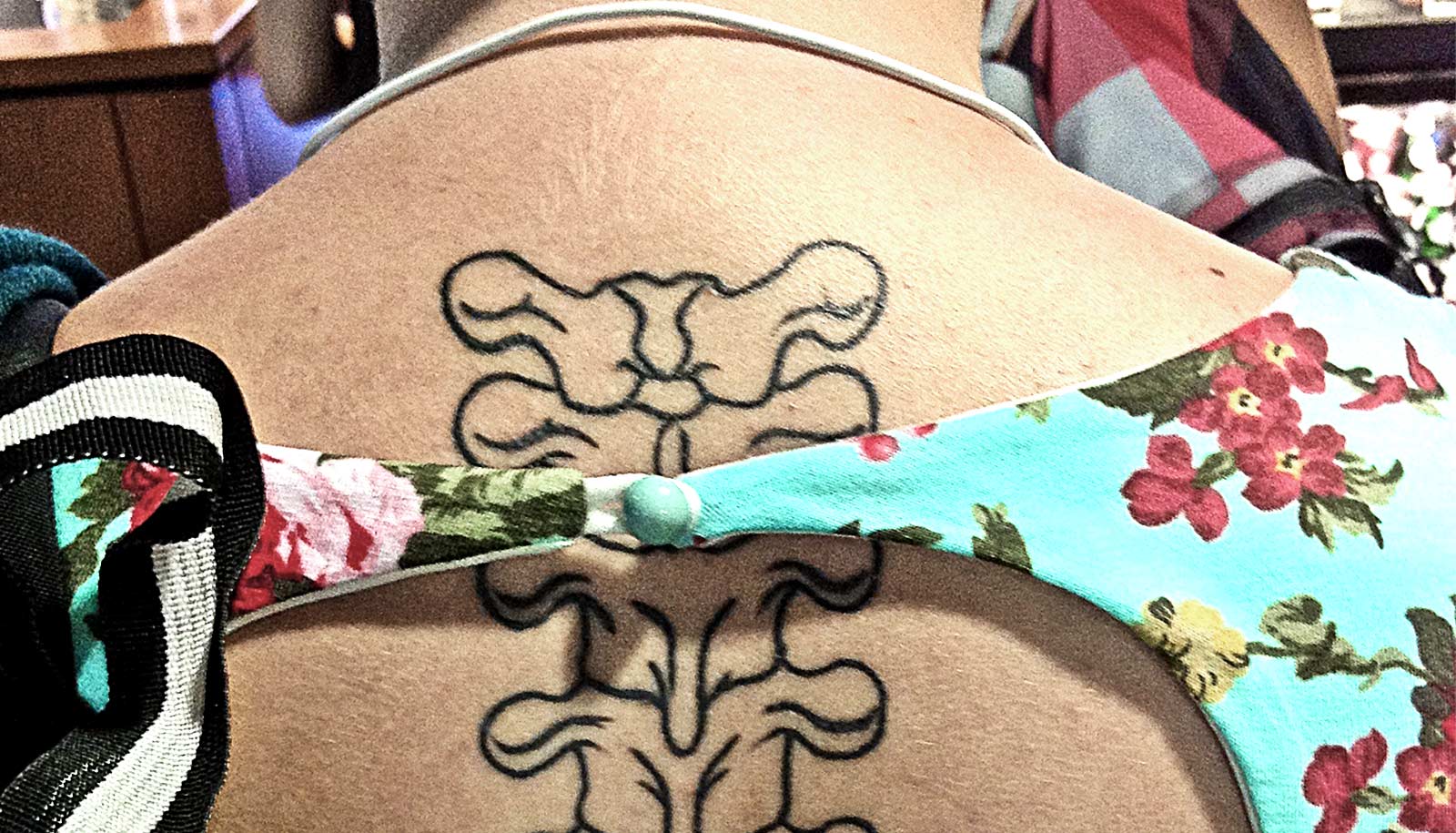
A major challenge for healing in such cases is the formation of glial scars that the cells and biochemicals that knit together around damaged nerves rapidly create. Initially the scarring offers a protective shield but over time it inhibits nerve repair.
“A glial scar is similar to other scars that form when you injure other parts of the body in that it protects the tissue from further damage, but glial scars don’t heal and remodel into healthy tissue like other scars typically do,” says Marian Hettiaratchi, an assistant professor at the Phil and Penny Knight Campus for Accelerating Scientific Impact at the University of Oregon.
“Chondroitinase ABC is a promising therapeutic protein, because it can degrade components of the glial scar, allowing healthy neurons to regrow.”
Natural chondroitinase ABC, she notes, loses most of its activity within 24 hours. The redesigned version is active for seven days. The enzyme was discovered two decades ago in the bacterium Proteus vulgaris. In animals, it has helped return lost function after severe spinal cord injury.
The natural enzyme is stable in its bacterial environment but once inside a body it is fragile, says senior author Molly Shoichet, a professor of chemical engineering at the University of Toronto.
“It aggregates, or clumps together, which causes it to lose activity,” Shoichet says. “This happens faster at body temperature than at room temperature. It is also difficult to deliver chondroitinase ABC because it is susceptible to chemical degradation and shear forces typically used in formulations.”
Various teams, including Shoichet’s, have experimented with techniques to overcome this instability. Some have tried wrapping the enzyme in biocompatible polymers or attaching it to nanoparticles to prevent it from aggregating. Others have tried infusing it into damaged tissue slowly and gradually, in order to ensure a consistent concentration at the injury site.
None of those approaches, however, addressed the instability.
In the new project, the research team altered the enzyme’s biochemical structure.
“Like any protein, chondroitinase ABC is made up of building blocks called amino acids,” Shoichet says. “We used computational chemistry to predict the effect of swapping out some building blocks for others, with a goal of increasing the overall stability while maintaining or improving the enzyme’s activity.”
The team had a lot of possible directions, says co-lead author Mathew O’Meara, a professor of computational medicine and bioinformatics at the University of Michigan.
To narrow down the search space, he says, the team applied computer algorithms that mimicked the types of amino acid substitutions found in real organisms. This approach, known as consensus design, produces mutant forms of the enzyme that don’t exist in nature but are plausibly like those that do.
In the end, the team ended up with three new candidate forms of the enzyme, but only one was both more stable and more active.
The next step will be to test the enzyme in the same kinds of experiments where the natural enzyme was previously used.
“This approach has not yet been used by tissue engineers interested in delivering therapeutic proteins for regenerative medicine,” Hettiaratchi says. “Since we’ve overcome one of the key challenges of using chondroitinase ABC, we hope that this will open new opportunities for the use of this enzyme as a therapeutic.”
The research appears in Science Advances.
Funding for the research came from the Natural Sciences and Engineering Council of Canada and the Canada First Research Excellence Fund.
Source: University of Oregon