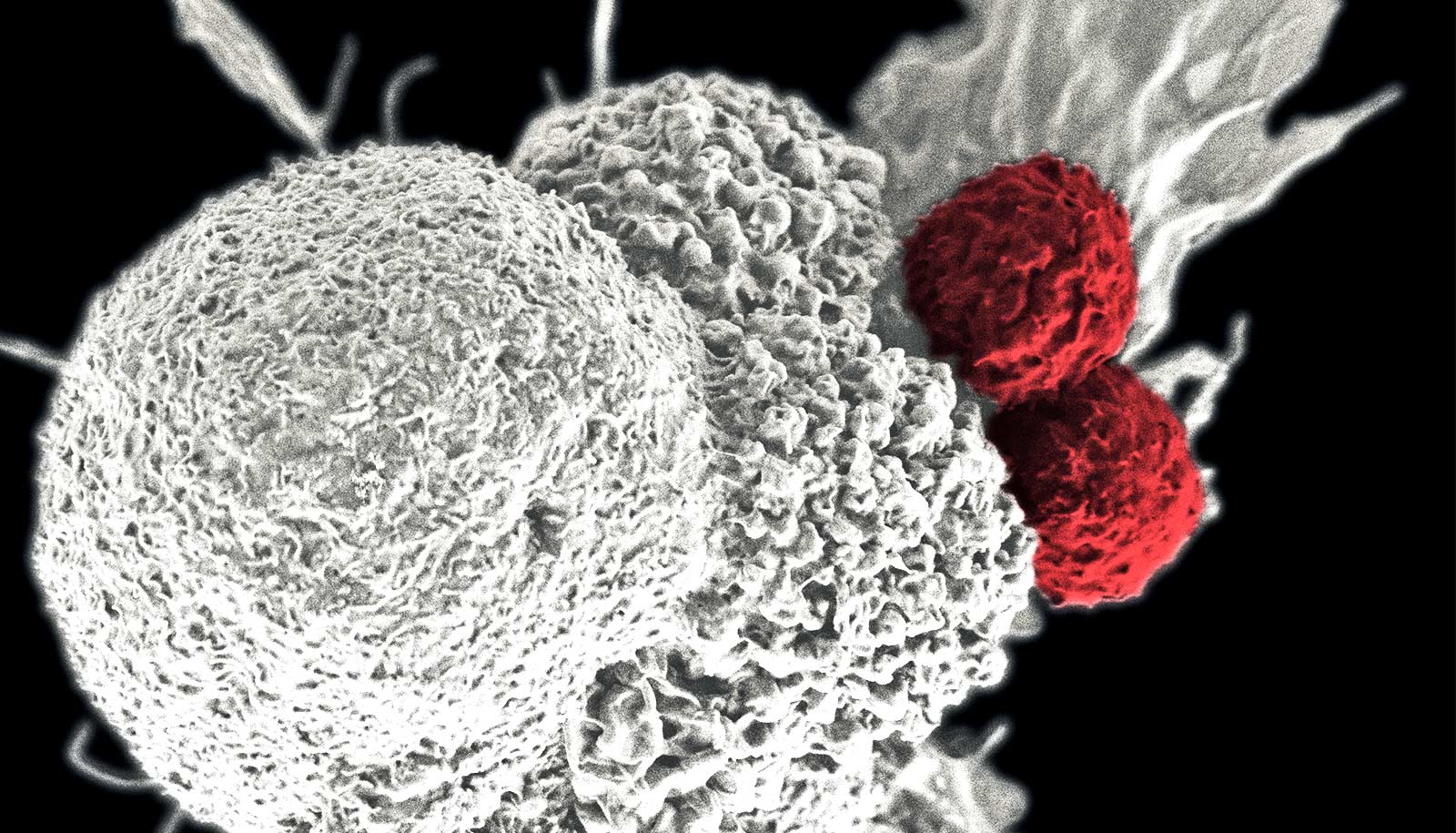
A drug treatment could improve the effectiveness of immunotherapy for cancer patients, researchers report.
“Immunotherapy has been one of the biggest breakthroughs in biomedical science and medicine of the last two decades. But it has limitations.”
The MDM2 gene promotes tumor growth and interferes with immunotherapy in some cancer patients.
The researchers’ new study in the journal Cell Death Discovery suggests that blocking MDM2 could bolster immunotherapy’s effectiveness.
Blocking MDM2 to boost cancer immunotherapy
While immunotherapy—a form of treatment that uses the body’s immune system to recognize, attack, and kill tumor cells—has given hope to people across the globe, it fails in a significant proportion of cancer patients.
“Immunotherapy has been one of the biggest breakthroughs in biomedical science and medicine of the last two decades,” says Wafik El-Deiry, a professor of pathology and laboratory medicine and associate dean for oncologic sciences at Brown University. “But it has limitations.”
Some people’s tumors respond to immunotherapy initially and then relapse. Other patients experience pseudoprogression, where tumors appear to grow before eventually shrinking. And a third group—between 5% and 29% of patients—experience hyperprogression, which means that immunotherapy actually worsens their tumor growth.
El-Deiry hopes that blocking MDM2, either through gene-silencing or the MDM2-inhibiting drug AMG-232, could be especially helpful for people with hyperprogression.
Too many MDM2 copies
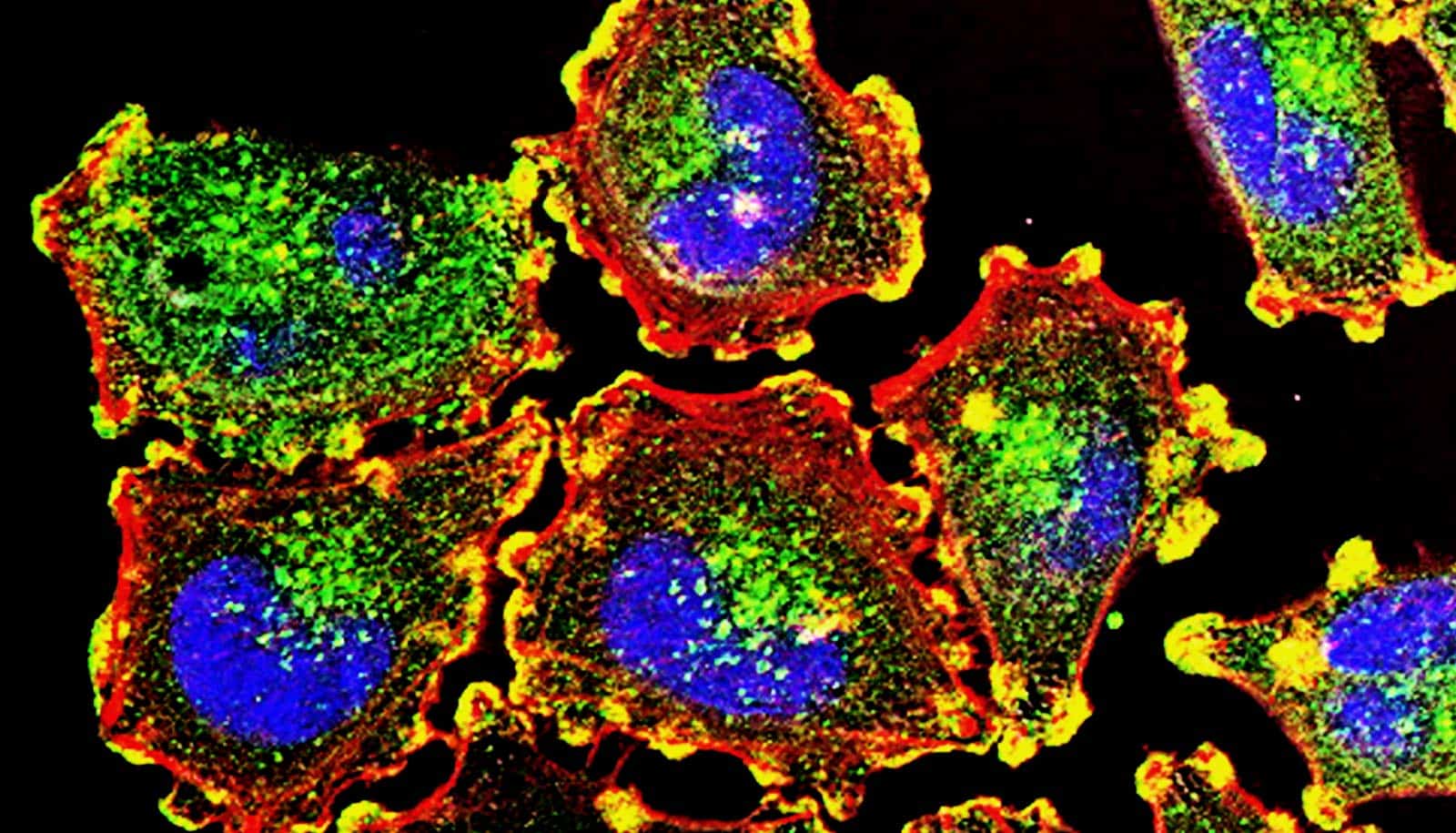
Various studies have found that when the MDM2 gene is amplified—meaning that cells contain too many copies of the gene—or when the MDM2 protein is overexpressed because the gene is not being regulated properly, tumor cells tend to grow more quickly and are more resistant to immunotherapy.
“It’s tapping into a vulnerability within tumors to help immunotherapy work better.”
Researchers are still investigating exactly why this accelerated growth and resistance occur, but studies suggest that MDM2 can help tumors grow and evade the immune system through a variety of mechanisms. For example, MDM2 appears to inactivate the tumor-suppressor gene p53 and prevent immune cells from killing tumor cells, and it is also associated with higher levels of a tumor-promoting inflammatory protein called interleukin-6 (IL-6).
In their study, El-Deiry and his colleagues treated cell lines of MDM2-overexpressing ovarian cancer cells with the therapeutic AMG-232. The data show that AMG-232 allowed immune cells to kill the tumor cells much more efficiently and reduced levels of IL-6.
These results suggest that MDM2 inhibitors could be combined with immunotherapy to enhance its effectiveness.
El-Deiry hopes the study will lead to a clinical trial so the research team can further evaluate the safety and effectiveness of this novel treatment. With MDM2 amplification and overexpression implicated in a variety of cancers, he believes that AMG-232 (or similar drugs, including those that block both MDM2 and a related protein, MDMX) could be widely applicable—and it could even benefit immunotherapy patients whose tumors have normal MDM2 levels.
“We think this might be a good approach to treat patients whose tumors are predicted to undergo hyperprogression, but I would say our results show that targeting MDM2 in combination with immunotherapy works well even if MDM2 is not amplified or overexpressed,” El-Deiry says.
“It’s tapping into a vulnerability within tumors to help immunotherapy work better,” he says.
The Mencoff Family endowed professorship at Brown supported the study.
Source: Kerry Benson for Brown University