A new anti-cancer drug has less toxic effects on the kidneys than current drugs do, researchers report.
The new drug works like a “magic bullet” that goes directly to cancer cells’ mitochondria—the power generators of cells. Once the drug reaches the tumor, two active molecules—an anti-cancer drug and a sensitizer—are released at once, where they attack the mitochondria, leading to the death of cancer cells.
The targeted approach reduces the drug’s interactions with other tissues, minimizing side effects. Researchers expect it to lower the risk of patients developing resistance to anti-cancer drugs like cisplatin.
The problem with current drugs
The discovery of cisplatin as an anti-cancer drug in 1965 was an important milestone that changed the treatment of the disease, and improved the cure rates of cancer patients worldwide.
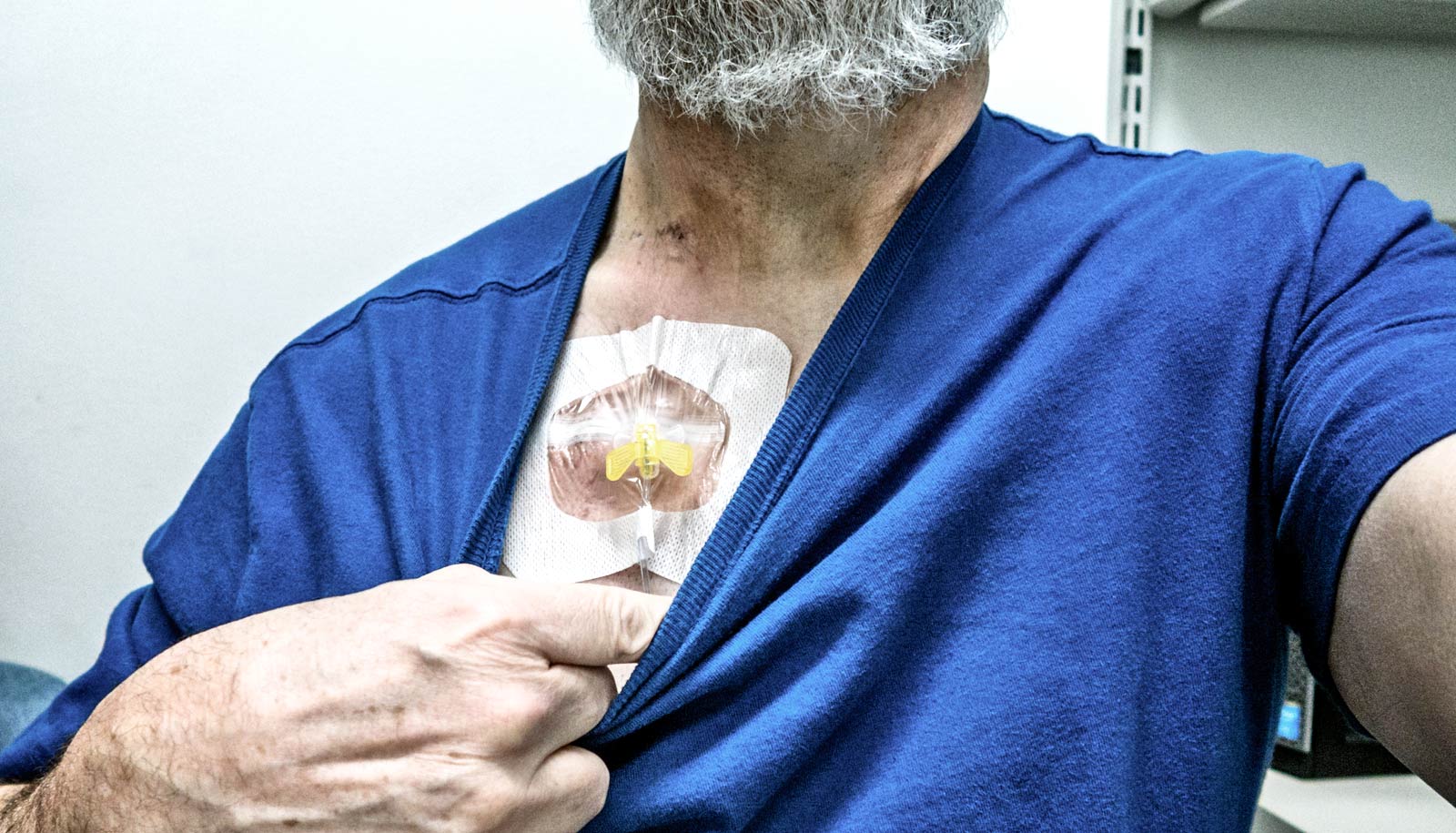
More than 50 years later, doctors still use cisplatin and the newer generation of platinum-based anti-cancer drugs in about 40% of all chemotherapy treatments. However, these drugs have toxic side effects, such as causing severe kidney dysfunction in patients, which may require some patients to undergo dialysis treatment.
“When designing and evaluating new cancer treatments, researchers often use cisplatin as a gold standard to compare new medicines. Cisplatin is known to kill cancer cells by damaging DNA. But cancer cells are smart, and they have ways to repair this damage and become resistant to the drug treatment. Hence, we need good alternatives that can address drug resistance and the associated side effects,” explains Ang Wee Han, an associate professor at the chemistry department at the National University of Singapore.
He worked together with Giorgia Pastorin, an associate professor in the pharmacy department, to look into developing an anti-cancer drug with better treatment outcomes to serve as an alternative to cisplatin.
Recognizing that the mitochondria have less efficient repair mechanisms in their DNA, the team came up with a novel drug that they could deliver directly to them. To do this, the researchers added a mitochondria-targeting ligand to the original cisplatin scaffold. This additional ligand has a strong positive charge that displays high affinity towards the complementary negative charge of the mitochondrial membrane.
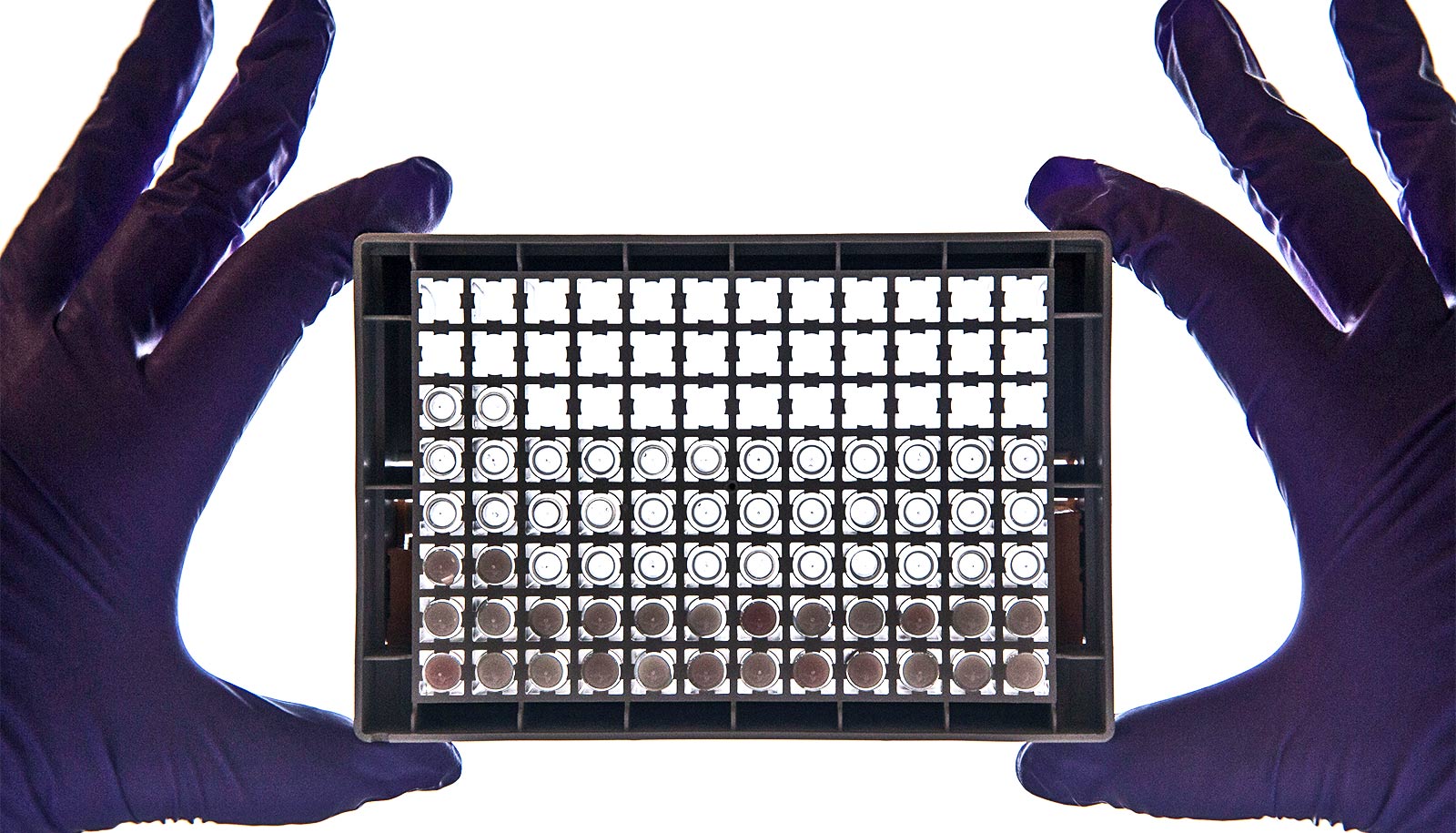
The researchers examined how their drug was released into the blood, and came up with a method to encapsulate the drug formulation in miniaturized drug carriers known as liposomal nanovesicles. As tumors grow very rapidly, their blood vessels do not have time to develop properly and are leaky. Such an environment enables the drug carriers to move from blood vessels to the tumor microenvironment and attack the cancer cells from within the tumor.
A better anti-cancer drug?
Experiments showed that when researchers delivered it to a colon cancer model the new drug shrank the tumor until it became impalpable.
“No sign of kidney inflammation was detected, unlike the use of conventional cisplatin. These results indicate that our invention is a viable alternative to cisplatin,” says first author Maria Babak, who is the first author of the study.
“While our results show great potential, we want to further challenge ourselves to improve our drug so that we can achieve complete tumor remission and tackle drug resistance. Accomplishing such a feat will open doors to improving cancer treatment and survival rates,” says Pastorin.
To improve the efficacy of the new drug, the researchers are looking into adjusting the doses and frequencies of the treatment. They are also studying combinations of different anti-cancer drugs, and examining ways to packaging them into suitable drug delivery systems to increase efficacy, decrease side effects and tackle drug resistance among cancer patients.
A paper on the drug appears in Angewandte Chemie International Edition. Dan Gibson from the Hebrew University of Jerusalem also contributed to the work.
Source: National University of Singapore