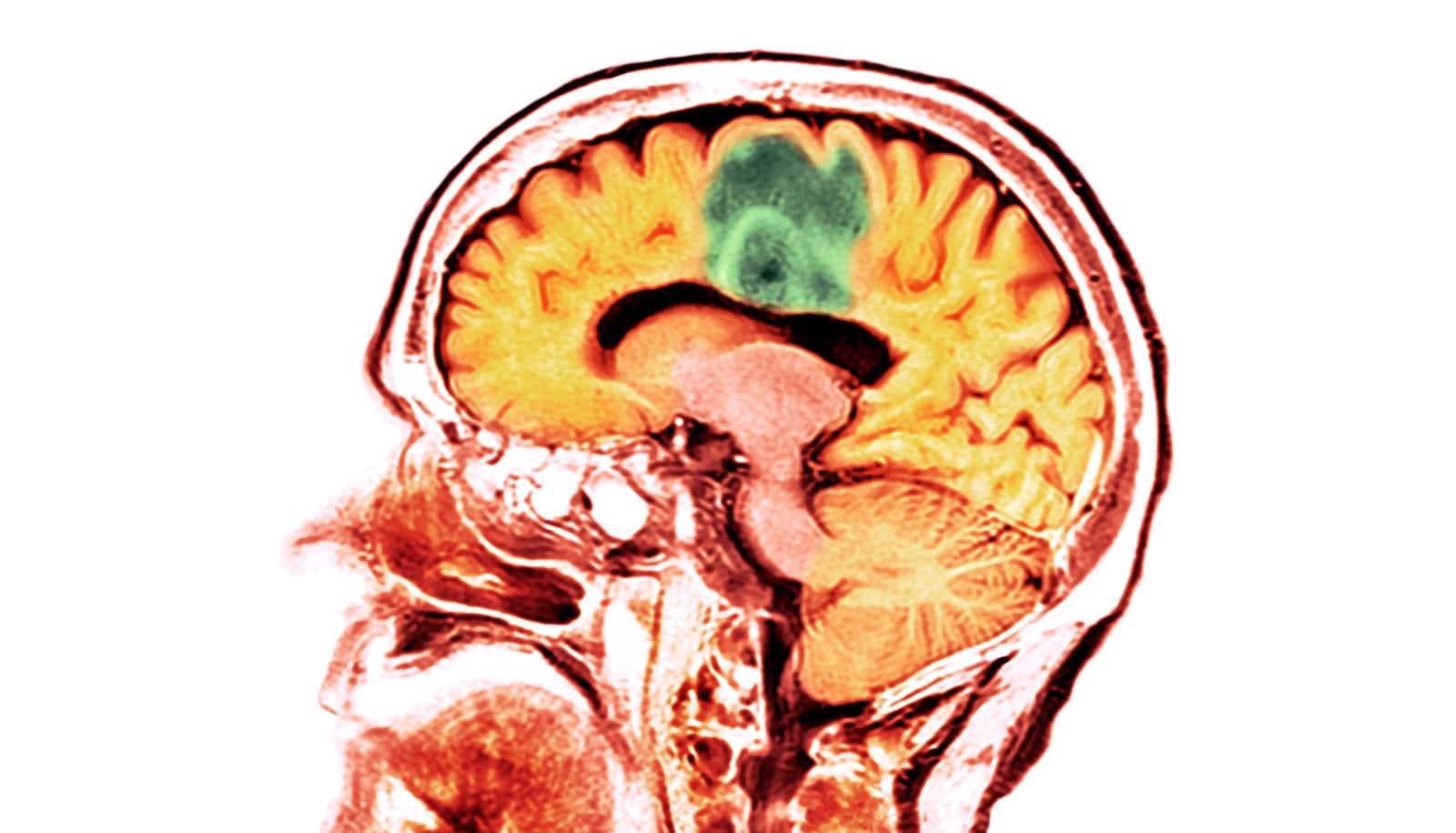
An intelligent molecule could significantly extend the lives of patients with glioblastoma, research finds.
Glioblastoma is an incurable and devastating brain cancer that affects people of all ages, regardless of their lifestyle.
The molecule, called ZR2002, which can be administered orally and is capable of penetrating the blood-brain barrier, could delay the multiplication of glioblastoma stem cells resistant to standard treatment.
The current average survival rate for glioblastoma is 15 months following diagnosis. Unfortunately, standard treatment, which has changed very little over the past 15 years, does not prevent the tumor from recurrence.
Sabotaging glioblastoma repairs
“Glioblastoma stem cells, which are extremely aggressive and highly resistant to the standard radiation and chemotherapy treatment Temodal, are believed to cause tumor recurrence. They have the ability to repair themselves when attacked with this treatment,” explains coauthor Bertrand Jean-Claude, senior scientist in the Metabolic Disorders and Complications Program at the Research Institute of the McGill University Health Centre (RI-MUHC).
“The ZR2002 molecule we developed is designed to kill two birds with one stone: on top of attacking the tumor, it destroys its defense system,” adds Jean-Claude, who is also the director and founder of the Drug Discovery Platform at the Centre for Translational Biology at the RI-MUHC.
Patients with glioblastoma usually undergo surgery to remove as much of the tumor as possible from the brain. To increase the chances of killing the remaining cancer cells, they then undergo six weeks of radiotherapy with chemotherapy followed by six months of chemotherapy treatment.
“In approximately 50% of glioblastoma patients, tumors carry a protein called EGFR that promotes the proliferation of tumor cells and makes them resistant to chemotherapy and radiotherapy,” says coauthor Bassam Abdulkarim, a radiation oncologist at the MUHC and senior scientist in the Cancer Research Program at the RI-MUHC.
“However, although the standard treatment is capable of damaging the DNA of cancer cells, it cannot circumvent the effects of EGFR. As a result, in many patients, the tumor grows back again while their treatment is still ongoing.”
The researchers designed the ZR2002 molecule to solve this problem. On one hand, it damages the tumor’s cellular DNA and, on the other hand, it irreversibly blocks the action of EGFR proteins.
Testing the ‘combi-molecule’
To test the efficacy of the new molecule, researchers had to establish glioblastoma stem cells resistant to the chemotherapy used for patient treatment. This is a complex task Janusz Rak, a senior scientist at the RI-MUHC and a professor in the pediatrics department at McGill, succeeded in performing.
“In an experimental mouse model, we subjected these highly aggressive and resistant stem cells to the action of the drug ZR2002,” says lead author Siham Sabri, a scientist in the Cancer Research Program at the RI-MUHC and assistant professor in the pathology department. “The results of the study show that when administered orally, ZR2002 induces anti-tumor activity significantly superior to that of Temodal and kills tumor cells through a multimodal mechanism of action.”
“The challenge is not only to fight the resistance of glioblastoma stem cells,” adds Abdulkarim, who is also a professor in the oncology department, “but also to deliver chemotherapy to the brain, which is protected by the blood-brain barrier. Our team has succeeded in meeting these two major challenges.”
To demonstrate that the orally administered molecule could cross the blood-brain barrier, the team used mass spectrometry imaging.
The researchers now hope to be able to continue their research and test this first-in-class combi-molecule in a clinical trial for patients diagnosed with glioblastoma.
The study appears in the journal Clinical Cancer Research.
Support for the study came from the Canadian Cancer Society Research Institute-Innovation, Cancer Research Society, the Canadian Institute of Health and Research, the Montreal General Hospital Foundation, McGill University Health Centre Foundation, and a donation from Susan Aberman and Louis Dzialowski through the Montreal Neurological Hospital Foundation.
Source: McGill University