A new proof-of-principle study shows a smartphone’s camera and flash can detect blood oxygen saturation levels down to 70%.
That’s the lowest value that pulse oximeters should be able to measure, as recommended by the US Food and Drug Administration.
When we breathe in, our lungs fill with oxygen, which is distributed to our red blood cells for transportation throughout our bodies. Our bodies need a lot of oxygen to function, and healthy people have at least 95% oxygen saturation all the time.
Conditions like asthma or COVID-19 make it harder for bodies to absorb oxygen from the lungs. This leads to oxygen saturation percentages that drop to 90% or below, an indication that medical attention is needed.
In a clinic, doctors monitor oxygen saturation using pulse oximeters—those clips you put over your fingertip or ear. But monitoring oxygen saturation at home multiple times a day could help patients keep an eye on COVID symptoms, for example.
The new technique involves participants placing their finger over the camera and flash of a smartphone, which uses a deep-learning algorithm to decipher the blood oxygen levels. When the team delivered a controlled mixture of nitrogen and oxygen to six subjects to artificially bring their blood oxygen levels down, the smartphone correctly predicted whether the subject had low blood oxygen levels 80% of the time.

“Other smartphone apps that do this were developed by asking people to hold their breath. But people get very uncomfortable and have to breathe after a minute or so, and that’s before their blood-oxygen levels have gone down far enough to represent the full range of clinically relevant data,” says co-lead author Jason Hoffman, a doctoral student in the Paul G. Allen School of Computer Science & Engineering at the University of Washington.
“With our test, we’re able to gather 15 minutes of data from each subject. Our data shows that smartphones could work well right in the critical threshold range.”
Another benefit of measuring blood oxygen levels on a smartphone is that almost everyone has one.
“This way you could have multiple measurements with your own device at either no cost or low cost,” says coauthor Matthew Thompson, professor of family medicine in the School of Medicine.
“In an ideal world, this information could be seamlessly transmitted to a doctor’s office. This would be really beneficial for telemedicine appointments or for triage nurses to be able to quickly determine whether patients need to go to the emergency department or if they can continue to rest at home and make an appointment with their primary care provider later.”
AI tracks blood oxygen levels
For the study, published in npj Digital Medicine, the team recruited six participants ranging in age from 20 to 34. Three identified as female, three identified as male. One participant identified as being African American, while the rest identified as being Caucasian.
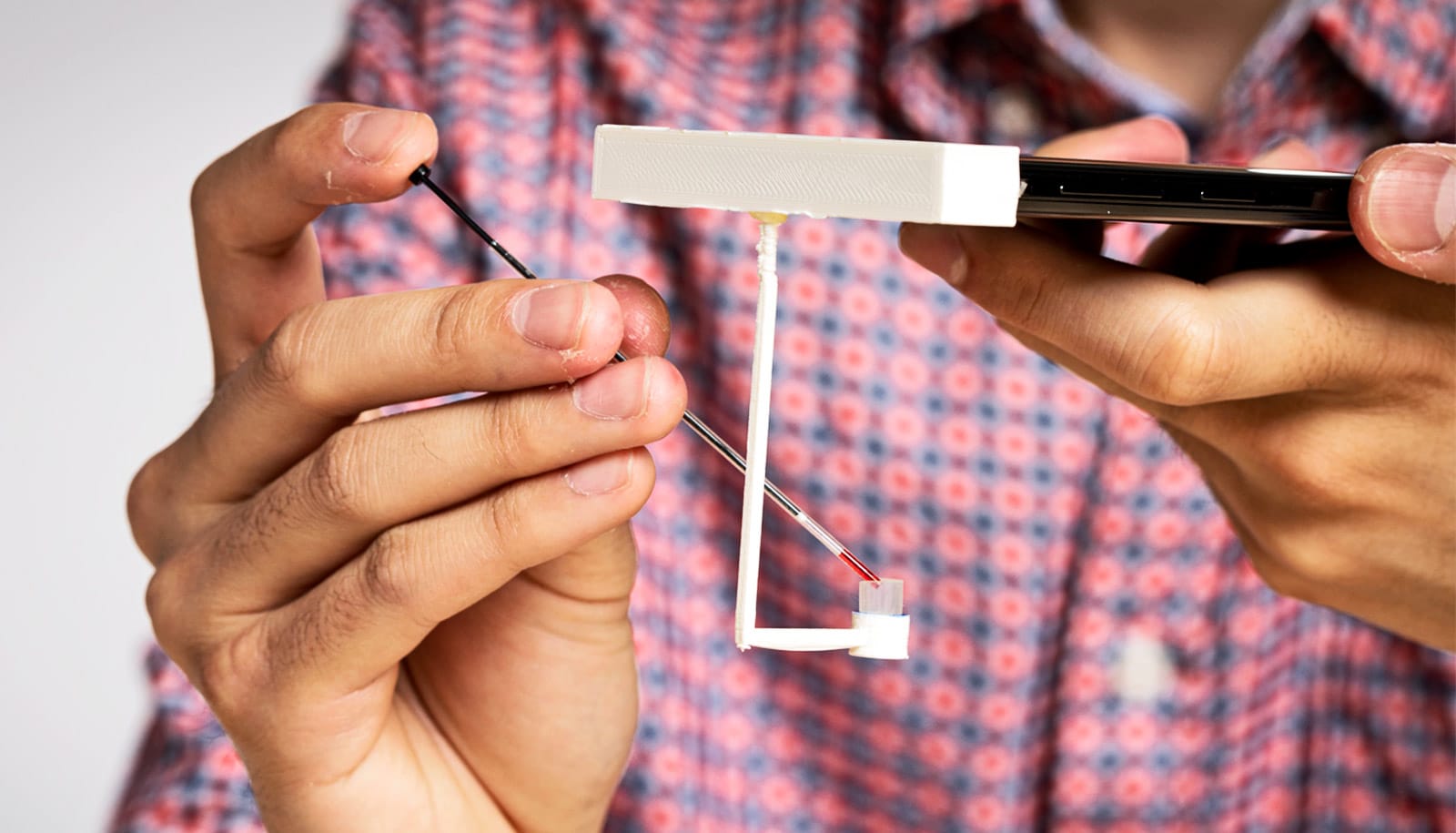
To gather data to train and test the algorithm, the researchers had each participant wear a standard pulse oximeter on one finger and then place another finger on the same hand over a smartphone’s camera and flash. Each participant had this same set up on both hands simultaneously.
“The camera is recording a video: Every time your heart beats, fresh blood flows through the part illuminated by the flash,” says senior author Edward Wang, who started this project as a University of Washington doctoral student studying electrical and computer engineering and is now an assistant professor at the University of California, San Diego.
“The camera records how much that blood absorbs the light from the flash in each of the three color channels it measures: red, green, and blue,” says Wang. “Then we can feed those intensity measurements into our deep-learning model.”
Each participant breathed in a controlled mixture of oxygen and nitrogen to slowly reduce oxygen levels. The process took about 15 minutes. For all six participants, the team acquired more than 10,000 blood oxygen level readings between 61% and 100%.
The researchers used data from four of the participants to train a deep learning algorithm to pull out the blood oxygen levels. The remainder of the data was used to validate the method and then test it to see how well it performed on new subjects.
“Smartphone light can get scattered by all these other components in your finger, which means there’s a lot of noise in the data that we’re looking at,” says co-lead author Varun Viswanath, a University of Washington alumnus who is now a doctoral student advised at UC San Diego.
“Deep learning is a really helpful technique here because it can see these really complex and nuanced features and helps you find patterns that you wouldn’t otherwise be able to see.”
Calluses and skin tones
The team hopes to continue this research by testing the algorithm on more people.
“One of our subjects had thick calluses on their fingers, which made it harder for our algorithm to accurately determine their blood oxygen levels,” Hoffman says.
“If we were to expand this study to more subjects, we would likely see more people with calluses and more people with different skin tones. Then we could potentially have an algorithm with enough complexity to be able to better model all these differences.”
But, the researchers say, this is a good first step toward developing biomedical devices that are aided by machine learning.
“It’s so important to do a study like this,” Wang says. “Traditional medical devices go through rigorous testing. But computer science research is still just starting to dig its teeth into using machine learning for biomedical device development and we’re all still learning. By forcing ourselves to be rigorous, we’re forcing ourselves to learn how to do things right.”
Additional coauthors are from Southern Methodist University and the University of Washington.
The University of Washington funded the work. The researchers have applied for a patent that covers systems and methods for SpO2 classification using smartphones.
Source: University of Washington