What happens when you stop using birth control? An expert weighs in on what to expect.
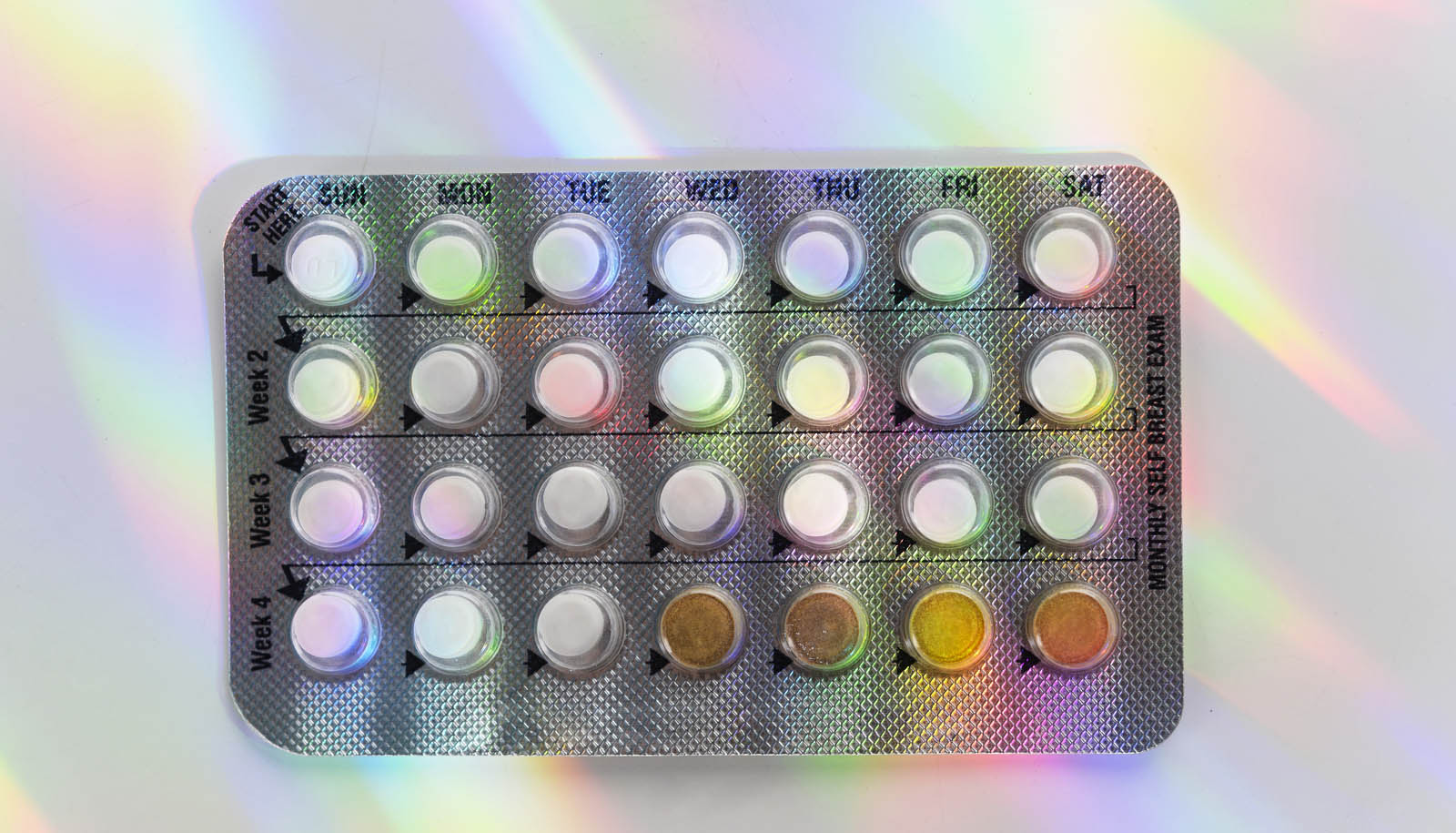
Of the more than 65% of women in the US between 15 and 49 using some type of contraception, nearly half turn to the pill, patch, ring, shot, or implant to prevent pregnancy, regulate hormones, or treat certain conditions.
If you’re one of them, you likely went through a few rounds of navigating side effects before finding the right one.
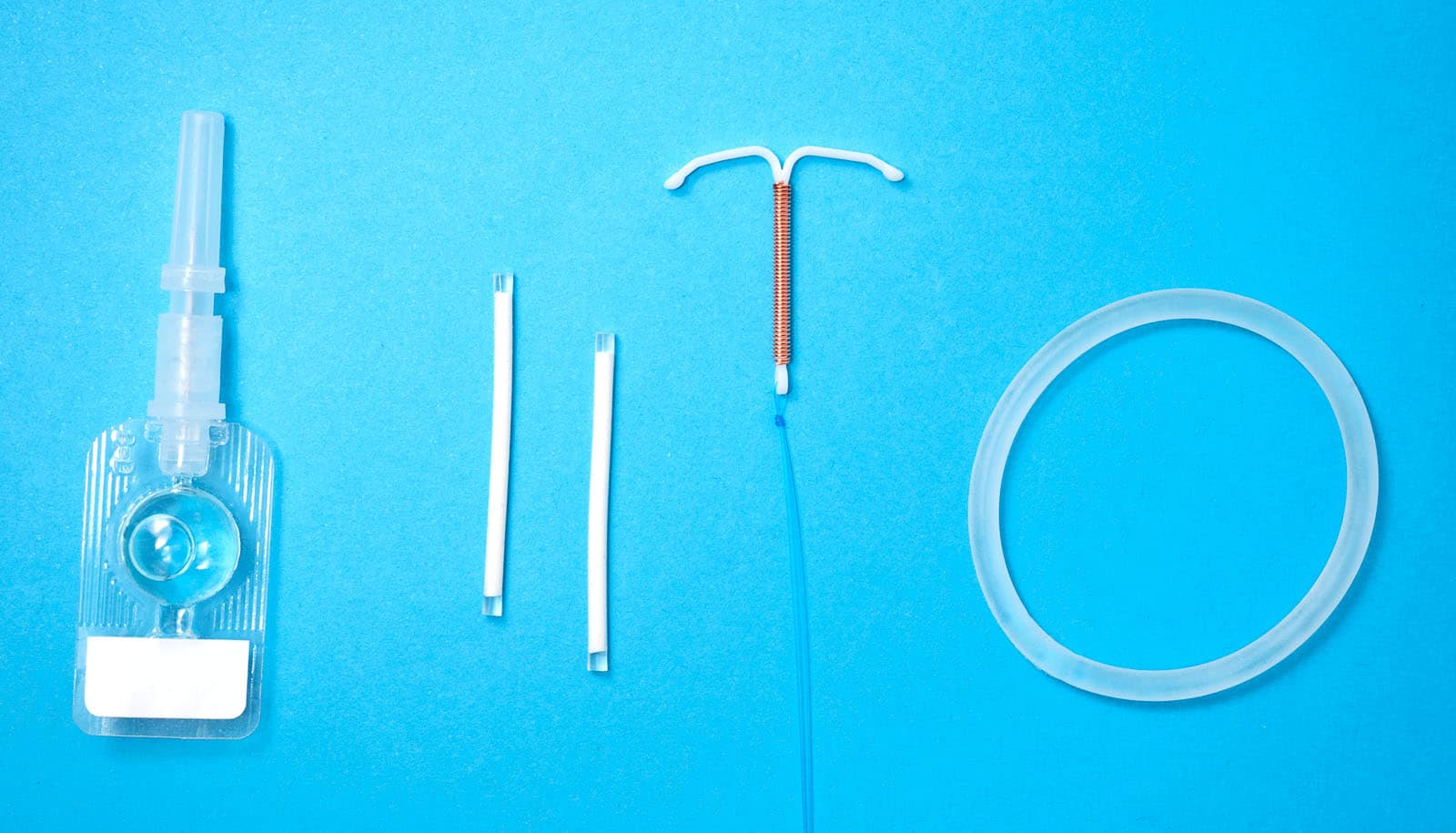
That’s because side effects of hormonal, non-hormonal, and long-acting reversible birth control (like IUDs) can range from barely there to downright debilitating, especially for those first few cycles on a new medication.
“The side effects differ from person to person,” says Stacy Sun, an assistant professor in obstetrics and gynecology at University of Rochester Medicine who specializes in complex family planning.
Some women may choose to stop birth control if their lifestyle changes, they want to get pregnant or regulate their period, or because they’re experiencing side effects. If your needs and priorities change, this is what you can expect when stopping birth control.
What does it feel like to stop the birth control pill, patch, or ring?
Many of these methods contain both estrogen and progesterone—Sun describes it as “a quiet, consistent level of hormones.” Without them, your body will automatically want to restimulate follicles to potentially ovulate.
The good news: these medications are fast going in and just as fast going out. Side effects from the medication such as headaches, mood changes, breast tenderness, or bloating will fade quickly.
Most people experience withdrawal bleeding within a week of stopping, which could feel like a light to normal period. Within three months, your cycles will likely return to their previous cadence.
If you experience any of the following symptoms after stopping, head to the nearest urgent care or emergency room:
- Heavy bleeding (using more than one pad per hour for two hours or more)
- Worsening dizziness
- Shortness of breath
What does it feel like to remove an intrauterine device (IUD) or implant?
IUDs and implanted devices (like Nexplanon) are inserted by a provider, so you will need to see them for removal. It’s a little more uncomfortable than simply stopping the pill: an IUD is removed via a speculum exam, while the implant is removed through a tiny incision in your arm.
Thankfully, the removal procedure is much more comfortable than the initial placement, and it takes less than 30 seconds. Pro tip from Sun: take ibuprofen or acetaminophen beforehand for pain. Self-removal is an option for IUDs, but not widely recommended.
Prepare to feel crampy and experience some spotting for 24 hours after removal. “It should just get better over time,” Sun says. “Every day should be a little better than the last.”
Nexplanon users may experience bruising at the removal site. If it becomes red, painful, or you develop a fever, contact your provider.
What does it feel like to stop the Depo-Provera shot?
While other birth control methods provide a steady stream of hormones, the shot is a large dose of progesterone all at once. That’s why it can take longer to return to normal ovulation—up to six months, Sun says—once you stop. The same goes for any side effects you may have from the medication, like headache and bloating.
You may experience irregular bleeding and spotting here and there as your body readjusts. Try not to worry—the “coming off” period may result in a more unpredictable bleeding pattern. Things should even out after three to six months.
Is there a right way to stop birth control?
If you’re on the pill, patch, or ring, the easiest and fastest way is to simply… stop. You don’t even need to ask a provider for permission, Sun says. “There’s no right or wrong way to stop it.” Simply don’t start your next pack of pills, insert the next ring, or apply another patch.
If you have an IUD, simply make an appointment to have it removed. If you’re receiving the Depo-Provera shot, just cancel your upcoming appointments.
Can I stop mid-cycle?
Yes! You can stop birth control, have your IUD removed, or stop getting the Depo-Provera shot at any time.
“If you’re taking the pill, patch, or ring, the cycle doesn’t actually exist. It’s on forever pause,” Sun says.
When will my cycle resume?
If you have an IUD removed or stop the Depo-Provera shot, you can expect your cycle to return in three to six months. Be sure to reach out to your provider if you experience heavy bleeding, pain that doesn’t get better, or persistent pain for a week after your removal.
If you were on the pill, patch, or ring, your cycle should resume within three months. If you haven’t had a cycle after three months after stopping, take a pregnancy test and see your provider for further care.
No matter what method you choose, the most important thing you can do when it comes to birth control is advocate for yourself.
“Listen to your body,” Sun says. “If something doesn’t feel right, call your provider.”
Source: Nina Elias for University of Rochester