Beneficial gut bacteria actively sense the mucus lining of the gut, using the information as a guide to stay in their proper place, new research shows.
Breakdowns in that communication can lead to abnormal bacterial behavior and gut inflammation.
The findings point to possible mechanisms behind intestinal conditions like Crohn’s disease and ulcerative colitis. They also suggest avenues to develop more effective probiotics.
A team of researchers led by University of Oregon microbiologist Jarrod Smith in the laboratory of biology professor Karen Guillemin report their findings in a paper in the journal Cell Host and Microbe.
“We often think of the mucus as a lubricant lining, kind of inert,” says Guillemin, a professor in the Institute of Molecular Biology. “But this work reveals that the bacteria are responding to particular chemical signals in the lining, and that can change bacterial physiology.”
A healthy gut microbiome is not just a matter of having a collection of specific microbes. It means having certain bacteria in the right places, at the right time, and behaving the right way. But mapping the spatial distribution and activities of gut bacteria is challenging in humans. Using zebrafish, which are transparent when young, researchers can watch how bacteria behave inside living animals.
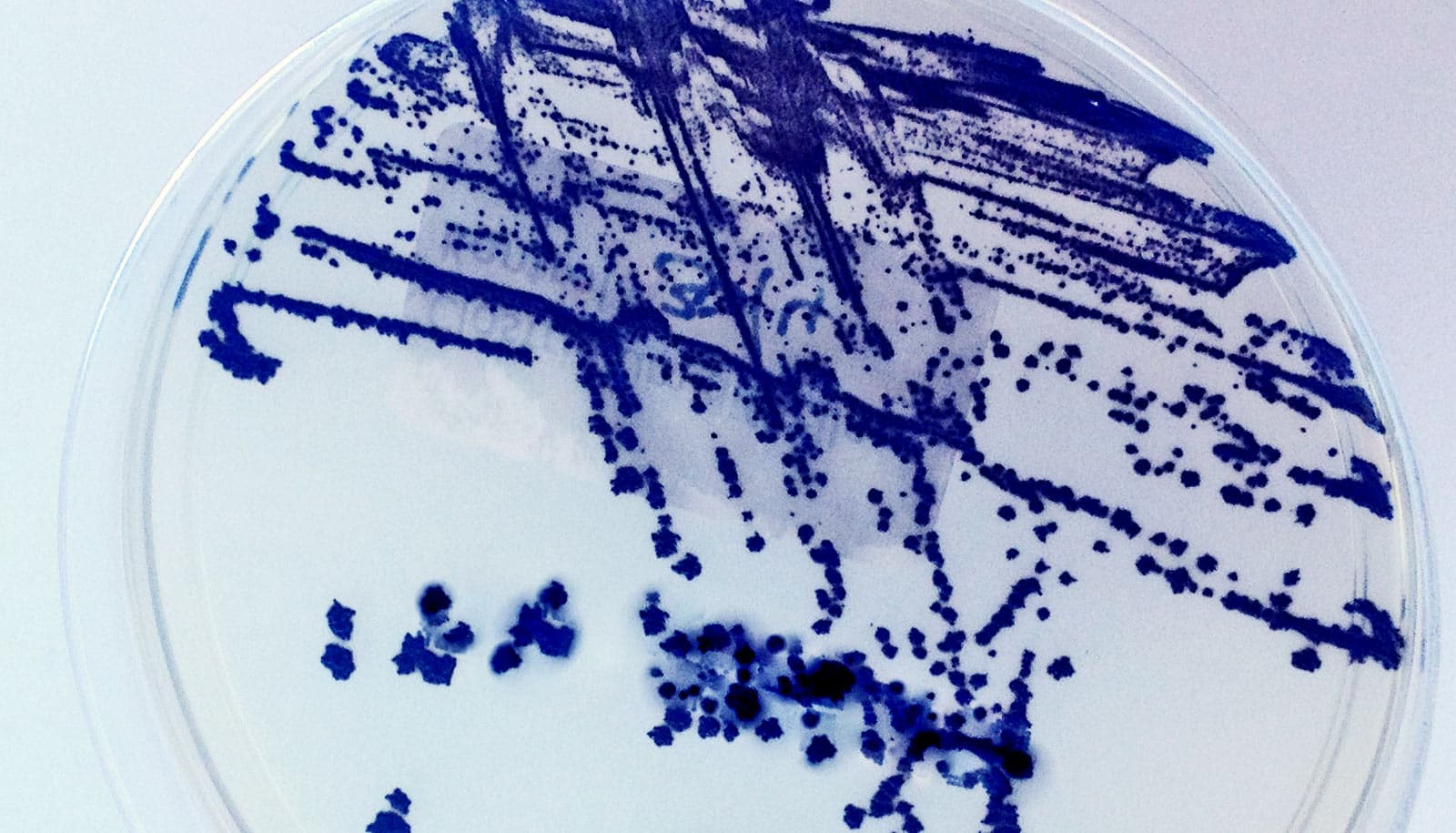
Guillemin’s team looked at Aeromonas bacteria, which are a key part of the zebrafish microbiome. In a healthy zebrafish gut, Aeromonas cells aggregate in large clumps in a specific region of the intestine.
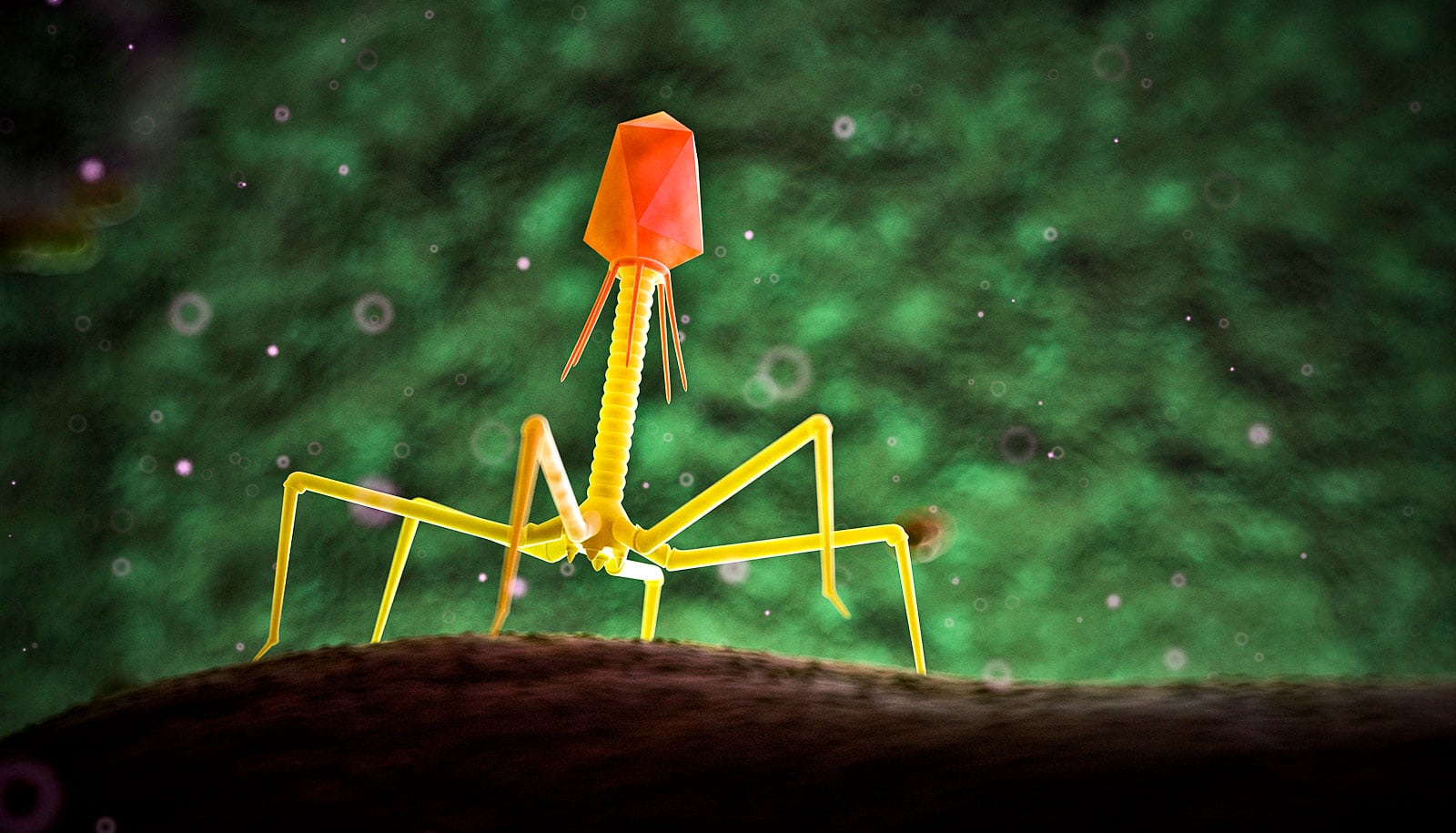
In the new study, the researchers identified a large protein on the surface of Aeromonas bacteria that detects gut mucus. Specifically, the protein interacts with glycans, complex sugar molecules that decorate the surface of the mucus proteins.
But Aeromonas bacteria engineered to lack that surface molecule didn’t congregate properly, the researchers showed. Instead of forming large aggregates, the bacteria operated as lone wolves and ended up in parts of the gut where they wouldn’t normally be. That, in turn, triggered inflammation.
The researchers could restore healthy bacterial behavior by engineering the Aeromonas bacteria to have a similar cell surface molecule sourced from a different bacterial species, Akkermansia muciniphila. Akkermansia are a beneficial kind of human gut bacteria that are sometimes found in probiotic supplements.
“What was broken in our bacteria was also found in a lot of human-associated bacteria,” Smith says. “Our data show that just by engineering a certain piece of one of these bacteria, you can reverse a lot of the inflammation.”
The finding suggests that communication between bacteria and gut mucus might be important across many species of bacteria, not just Aeromonas. Understanding specifically how beneficial bacteria are behaving in the gut—and what’s gone wrong when they don’t pick up on the contextual cues to behave properly—could help scientists develop more evidence-backed probiotic formulations that target specific issues.
The research also provides a new model for studying gut inflammation. Intestinal conditions like Crohn’s, colitis, and irritable bowel syndrome are poorly understood, so having different ways to model inflammation in the lab can help researchers get to the root of those complicated conditions.
“For me, a major takeaway from this study is that it provides new ideas about how we expect beneficial bacteria to behave in a healthy gut, and the molecular mechanisms that promote these health-associated behaviors,” Guillemin says.
Funding for this research came the National Institutes of Health.
Source: University of Oregon