A pilot study has found evidence of Bartonella infection in the blood of people with schizophrenia and schizoaffective disorder.
“Researchers have been looking at the connection between bacterial infection and neuropsychiatric disease for some time,” says first author Erin Lashnits, a former veterinary internist at North Carolina State University and current faculty member at the University of Wisconsin.
“Specifically, there has been research suggesting that cat ownership is associated with schizophrenia due to the zoonotic parasite Toxoplasma gondii, but to date there has been no conclusive evidence in support of a causative role for this parasite. So we decided to look at another cat-associated infectious agent, Bartonella, to see if there could be a connection.”
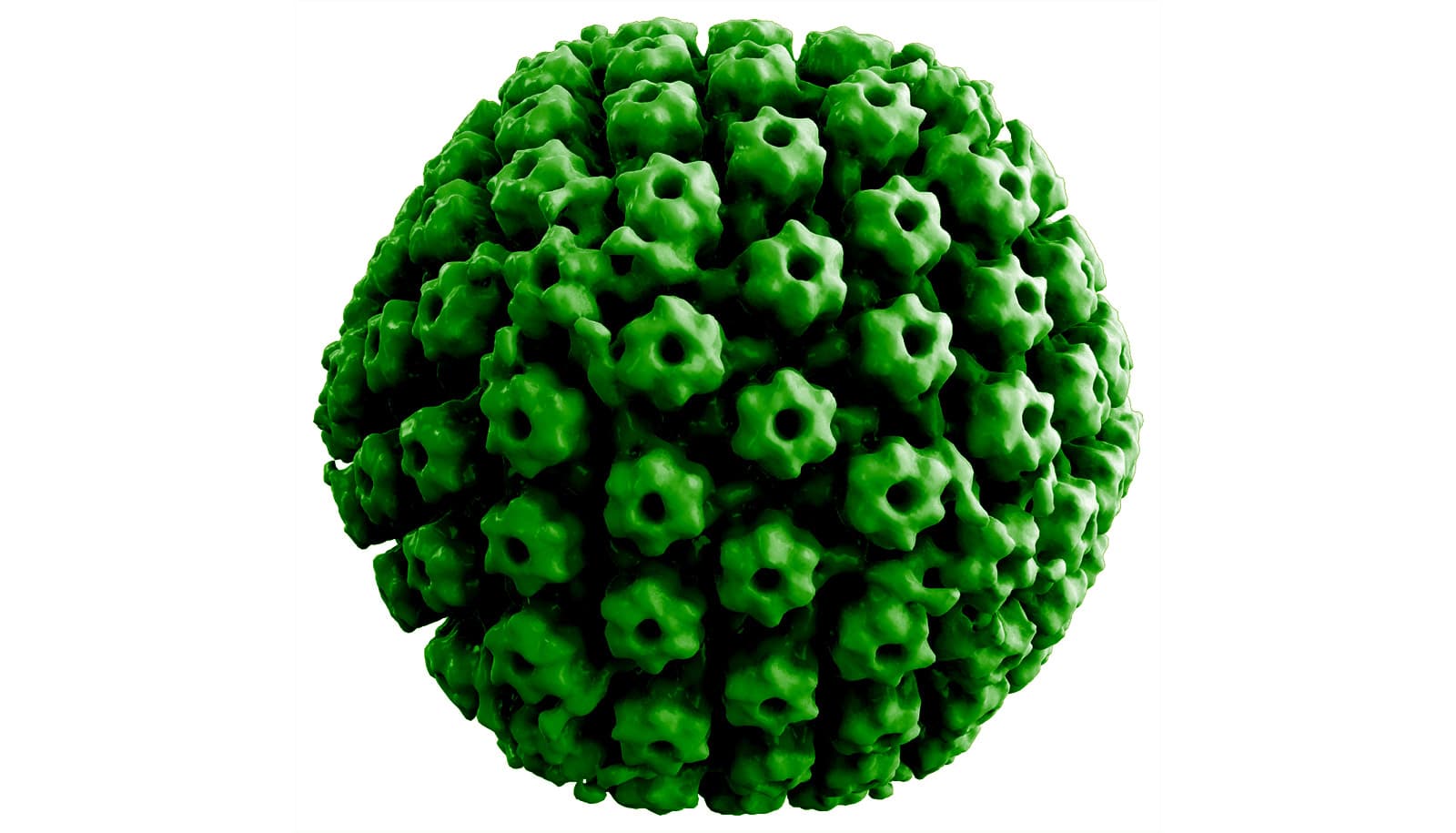
Bartonella are bacteria historically associated with cat-scratch disease, which until recently was thought to be solely a short-lived (or self-limiting) infection. Cats can become infected with Bartonella via exposure to fleas and potentially ticks, which are natural vectors of the bacteria. The cat is a host for at least three of the 40 known Bartonella species: Bartonella henselae, Bartonella clarridgeiae, and Bartonella koehlerae.
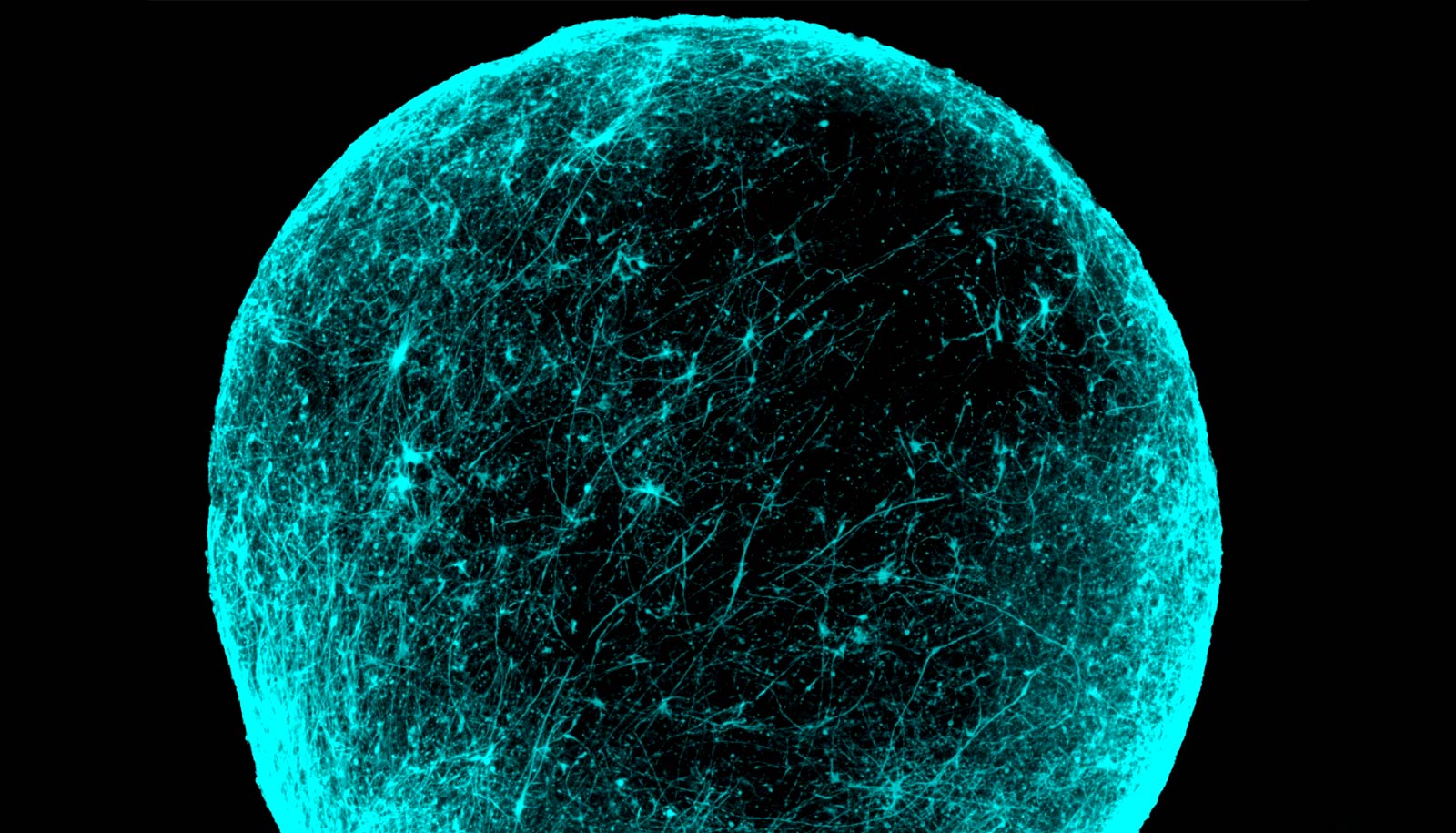
“While there is emerging understanding of neuropsychiatric illnesses such as schizophrenia as disorders of brain networks, the question about the actual causes remains unanswered,” says Flavio Frohlich, associate professor of psychiatry at the UNC School of Medicine, and corresponding author of the paper in Vector Borne and Zoonotic Diseases.
“To our knowledge, this is the very first work that examines a potential role of Bartonella in schizophrenia,” Frohlich says.
The research team enrolled a group of 17 people with stable, medically managed schizophrenia or schizoaffective disorder, and a control group of 13 healthy adults, to test for evidence of Bartonella infection.
All participants filled out questionnaires on severity of symptoms and potential Bartonella exposure. Researchers took blood samples from participants twice in a one-week period. They then cultured the samples in a growth medium, and both cultured and whole blood samples underwent qPCR and droplet digital, or ddPCR testing, at seven-, 14- and 21-day intervals, to look for evidence of Bartonella organism-specific DNA. The researchers also tested blood samples for Bartonella species-specific antibodies.
Of the 17 patients with schizophrenia, 12 had Bartonella DNA in their blood, as compared to only one of 13 in the control group. According to the questionnaires, both patients and controls reported similar pet ownership and flea exposures.
“Bartonella ddPCR, a very new diagnostic technology, provides a more sensitive molecular test than we’ve previously had access to,” says coauthor Ed Breitschwerdt, professor of internal medicine. “If we had not used ddPCR to test this cohort of individuals, we would not have found Bartonella DNA in any of the participants, either case or control.”
“It is important to remember that our study was by design not able to demonstrate a causal link between Bartonella infection and schizophrenia,” Frohlich says. “However, we believe this initial observational study strongly supports the need for follow-up research.”
The researchers plan to proceed with a larger study to see whether their preliminary results are borne out.
“Many of these patients have been undergoing care for years,” Breitschwerdt says. “What we’re starting to see is a pattern—Bartonella can persist for a long time. And for the subset of people who can’t eliminate the infection, the bacteria can cause chronic or progressive illness.”
The National Institutes of Health supported the work.
Source: NC State