Scientists have previously overlooked the astonishing physical strength of the thin outer membrane that clings to E. coli‘s stout cell wall, according to a new study.
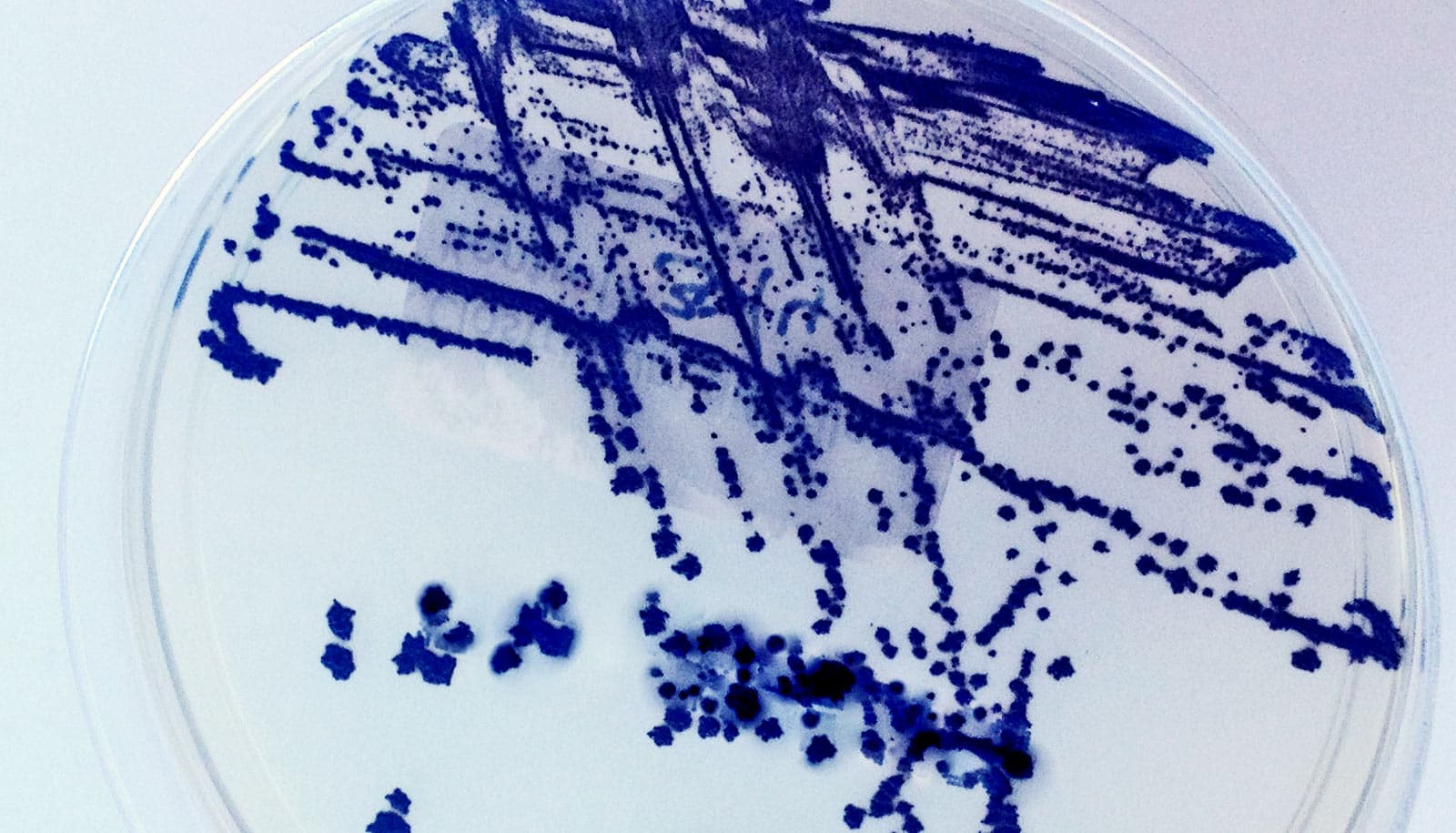
For over a century, scientists have studied E. coli, one of the bacteria that cause food poisoning, as a model for fighting infections. Such research has led to a variety of antibiotics that penetrate the protective cell walls of bacteria to kill them.
The new research, however, reveals that E. coli has managed to keep a big secret about its defenses.
Scientists had long known that many bacteria have outer membranes. But until now researchers thought of it like a layer of shrink wrap that simply made it tougher to get antibiotics into cells. But as the new study shows, the outer membrane physically protects the cell and could be a good target for a new class of antibacterial drugs.
“We’ve discovered that the outer membrane can act as a suit of armor that is actually stronger than the cell wall,” says K. C. Huang, an associate professor of bioengineering and of microbiology and immunology at Stanford University. “It’s humbling to think that this function had been hiding in plain sight for all these years.”
Huang says the findings suggest new infection-fighting strategies for the roughly half of all bacterial species that, like E. coli, have outer membranes.
“If we can attack the outer membrane, infectious bacteria will be pre-weakened for targeting with antibiotic treatments that disrupt cells in other ways,” he says.
Behind the shield
All bacteria have a cell wall that surrounds and protects the cell’s inner workings. Many decades ago, scientists discovered that E. coli and many other bacteria have an additional layer, called an outer membrane, that surrounds their cell walls.
Since its discovery, this outer membrane has been used as a way to classify bacteria into those that do and do not react to a common staining technique, called a Gram stain. Bacteria with outer membranes do not react to the chemical stain are called Gram-negative. Bacteria with naked cell walls react to the stain and are classified as Gram-positive.
Both kinds of bacteria can become infectious and, when this occurs, the presence or absence of an outer membrane can also help determine how responsive they will be to antibiotics. Gram-negative bacteria—which have outer membranes—tend to be more resistant to antibiotics.
“Scientists knew that outer membranes were chemical shields,” Huang says. “Thus, it was easy to relegate this third layer to an annoyance when dosing the cell with antibiotics.”
Tests of strength
In recent years, however, researchers have had clues that the outer membrane is more important than they’d thought. In one study, Huang’s lab removed E. coli‘s cell wall but left its outer membrane intact. Unsurprisingly, the bacteria lost their cucumber shape and became blobs. But a large fraction of these blobs survived, multiplied and ultimately regenerated new cucumber-shaped E. coli.
“…a strong outer membrane is the difference between life and death…”
Enrique Rojas, a former postdoctoral scholar in Huang’s lab and first author of the new paper, says that study was a clue that the outer membrane must play important structural and protective roles.
“We just listened to the data. Science is about data, not dogma,” says Rojas, now an assistant professor of biology at New York University.
Over the last four years, the group members tested the outer membrane’s structural powers.
They suddenly collapsed the pressure inside the bacteria, but instead of causing the cell wall to massively shrink, as prevailing assumptions would have predicted, they found that the outer membrane was strong enough to almost entirely maintain E. coli‘s cucumber shape.
In other experiments, they put E. coli cells through two hours of rapid increases and decreases in pressure. E. coli cells normally shrug off these repeated insults and grow as if no changes at all had occurred. However, when the researchers weakened the outer membrane, cells died quickly.
‘Smart antibiotics’ kill C. diff and spare good bacteria
“The presence or absence of a strong outer membrane is the difference between life and death,” Huang says.
The experiments identified a handful of components that give the outer membrane its surprising strength. Drugs that destabilize the deceptively thin outer layer could help destroy infectious bacteria, Huang says.
New insights
Huang adds that the findings are part of an emerging field of study called mechanobiology. Whereas scientists once viewed cells as sacks of chemicals to study by chemical means, today a confluence of tools reveal the infinitely complex structural properties that make cells and organs tick.
“It’s a very exciting time to be studying biology,” Huang says. “We are approaching the point at which our tools and techniques are becoming precise enough to discern, sometimes at almost the atomic level, the physical rules that give rise to life.”
Watch how bacteria ‘harpoon’ DNA to develop drug resistance
The research appears in Nature.
Additional coauthors are from Stanford; the University of California, San Francisco; and the University of Wisconsin-Madison.
Funding for the research came from the National Institutes of Health; the National Science Foundation; the Stanford Systems Biology Center and Simbios Center for Physics-Based Computation at Stanford; the Howard Hughes Medical Institute; the Swiss National Science Foundation; and the Allen Discovery Center program through the Paul G. Allen Frontiers Group.
Source: Stanford University