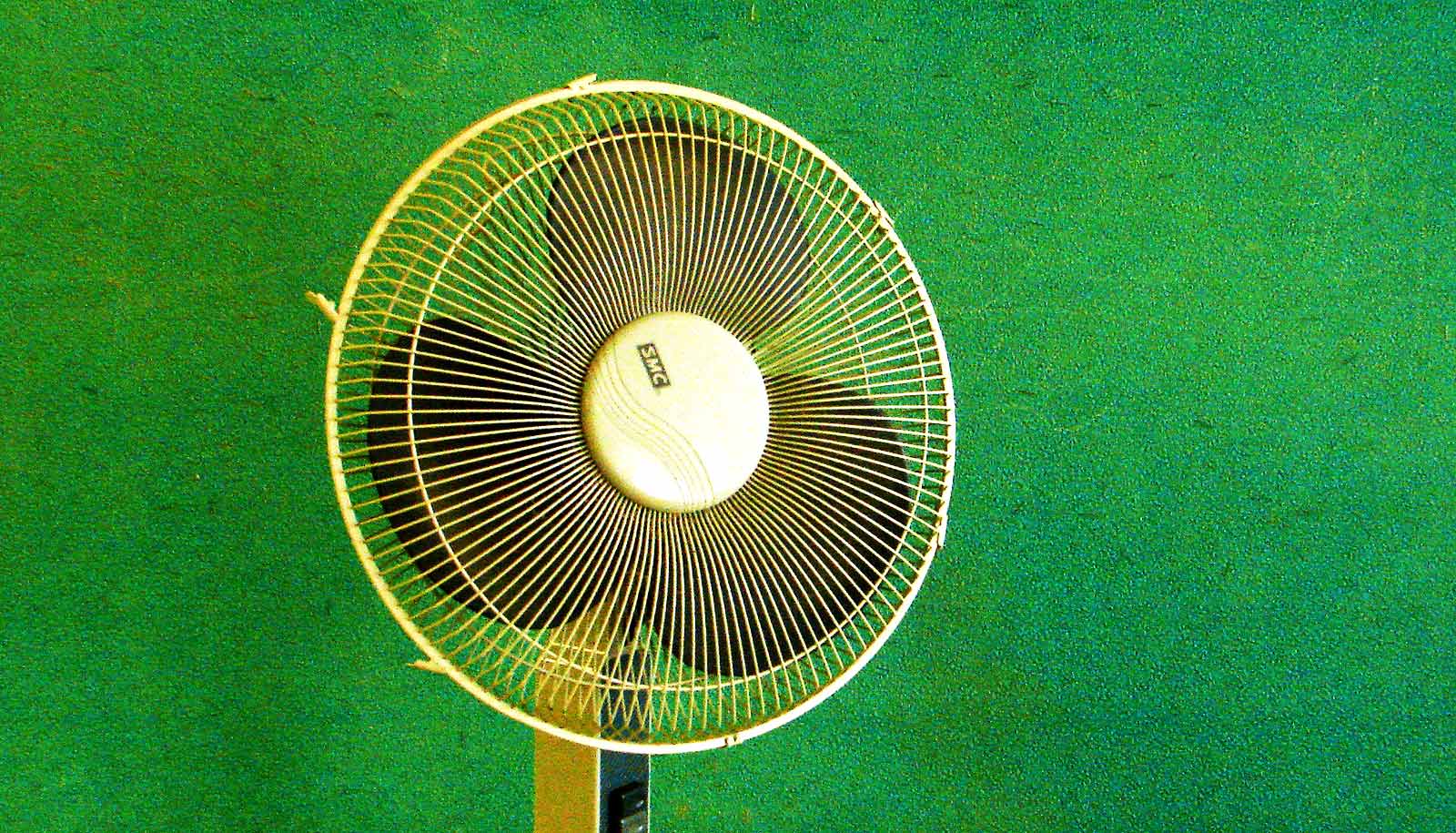
Air circulation and ventilation is key to preventing a build-up of droplets and aerosols that spread COVID-19, researchers say.
Most COVID guidelines have stressed the 6-foot physical distancing rule, with the idea being that the virus spreads through large droplets produced when we talk, cough, or sneeze. Relatively heavy, these droplets tend to fall to the ground before they travel more than a few feet.
“…the concentration of these droplets and aerosols are actually building up over time in a confined space.”
“However we are having these outbreaks even when people are keeping this 6-foot distance, and especially indoors,” says Bjorn Birnir, the director of the Center for Complex and Nonlinear Science at the University of California, Santa Barbara. More recent evidence suggests that the virus also travels in smaller droplets and aerosols, which can linger in the air for hours.
Birnir and his colleague Luiza Angheluta—a professor at the University of Oslo and currently a visiting researcher at the Kavli Institute for Theoretical Physics—decided to apply their expertise in fluid dynamics to COVID super-spreading events to understand how they might have happened. The crucial factor, they found, was air circulation.
Their results appear on medRxiv, the preprint server for health sciences, and are currently undergoing peer review.
In late January and early February, 10 individuals from three families all fell ill after eating at the same air-conditioned restaurant in Guangzhou, China on Chinese New Year. The cases all were linked to a single contagious customer at the restaurant.
All the diners who came down with the infection sat in one section of the restaurant, which was served by a single air conditioning unit. Patrons at another table close to the infected person, but under the breeze of a different AC unit, did not become ill.

The topic Birnir studies seemed perfect for understanding what happened at the restaurant. He specializes in fluid dynamics and was working on a class of problems called Lagrangian fluid dynamics, which involves following a fluid’s flow.
“This is exactly what you want to do with these droplets and aerosols,” he says. “You want to follow them, and you want to see where they go.”
Fittingly, Birnir had just made significant progress in in this domain in January.
Fluid flow is random and irregular, so mathematicians don’t try to capture all the details. Instead, they take statistical averages of the total fluid flow over a period of time. This technique allowed Birnir and Angheluta to build a model of how the flow carries around particles, which are called “passive scalars” because they are carried by the flow, but don’t influence it.
“What we discovered was that the concentration of these droplets and aerosols are actually building up over time in a confined space,” he says. This contrasted sharply with the belief that infectious droplets were large and would just settle out of the air.
After 15 minutes in an unventilated room the size of that section of the restaurant, a person anywhere would experience the same effects as if they had been sitting next to the contagious individual. “And in an hour, it’s four times what you would get if you were initially sitting next to the infected person,” Birnir says.
Many people had assumed that air conditioning would mitigate this issue. Namely, that the combination of the AC filter and the intake of outside air would be enough to keep viral loads in check.
The researchers found, however, that normal air conditioning only delayed the particle buildup in the restaurant by 10 minutes, and decreased the one-hour exposure rate to 2.5 times what it would have been initially right next to the contagious person.
“Basically, our conclusion is that these super spreaders are not really people, they are air conditioning and recirculating air flow in confined spaces,” Birnir says.
If the HVAC system isn’t taking in 100% new air, and doesn’t have high-quality filters, the concentration of small droplets and aerosols, and thus virus particles, will likely build up over time.
This has major implications for how we approach risk management in offices and classrooms.
“The good news is that we have a way of combating this virus, which we didn’t realize,” Birnir says. “It’s ventilation.”
Good ventilation, accredited filters, and face coverings can help reduce infection rates. In fact, people applied similar strategies to good effect when tackling tuberculosis in the days before antibiotics, Birnir says.
But most office and apartment AC units simply aren’t strong enough to handle the better filters and increased airflow, he says. “We need a new generation of air conditioners for the spaces where people spend most of their time.”
Birnir is currently advising the university’s administration as it develops plans and protocols for the coming academic year.
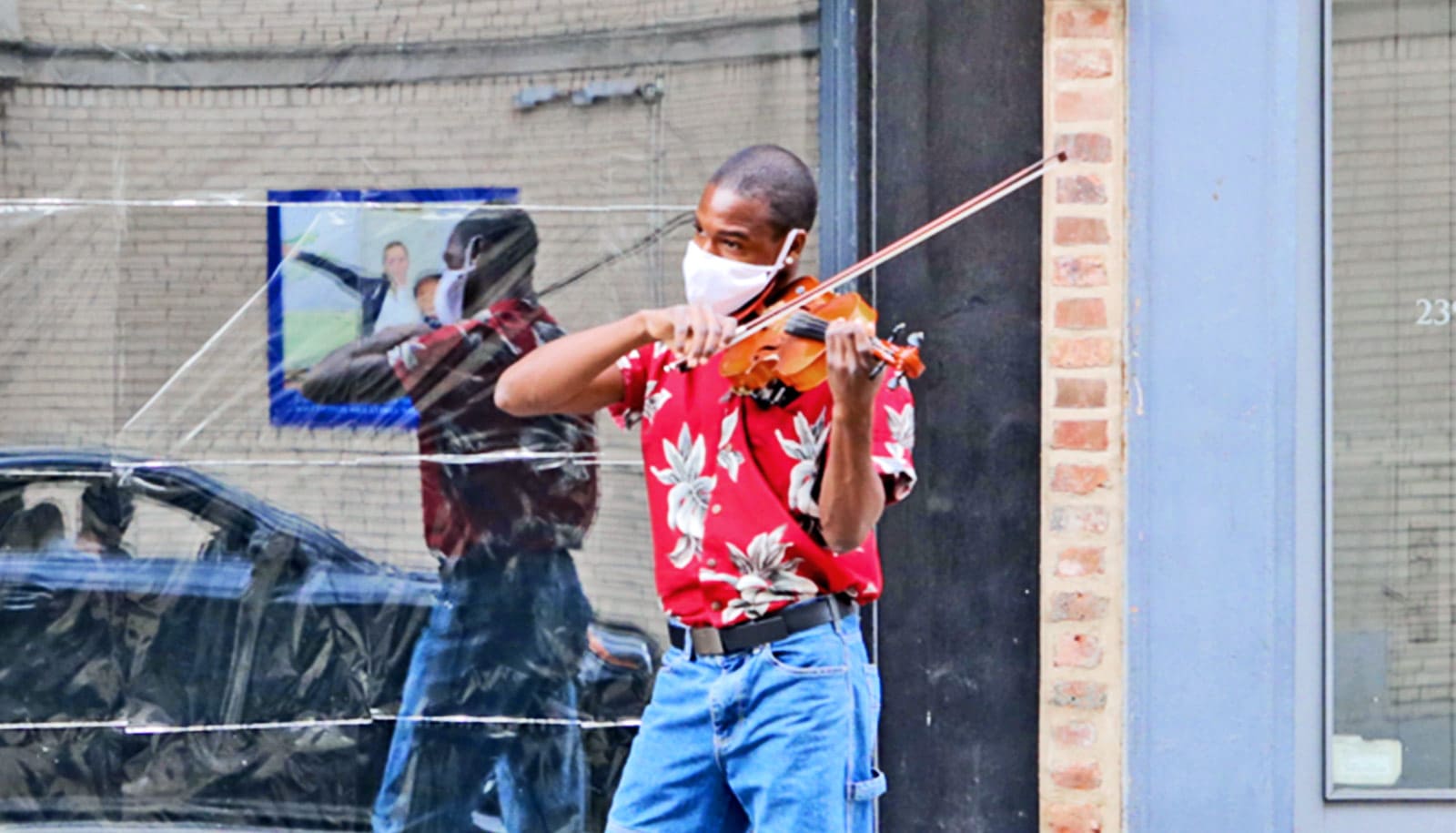
“If we start to allow some in-person classes, we may want to have them outside,” he says. “Because we always have a little bit of a breeze in Santa Barbara, and that’s all you need. If you have classes with physical distancing—so you can’t be infected by big droplets—and you have a little bit of a breeze going through, then you have a safe space.”
Source: UC Santa Barbara