A review of the Brazilian health system finds that women have a 90% increased risk for prescription combinations known to produce dangerous reactions.
The analysis, which appears in the journal npj Digital Medicine, reveals a 60% increased risk for adverse drug reactions in women compared to men—and a 90% increased risk in cases of medicines whose interaction is known to produce dangerous reactions. In older people, one in every four people prescribed multiple medicines over age 55 received drugs with an interaction—reaching one in every three for ages 70 to 79.
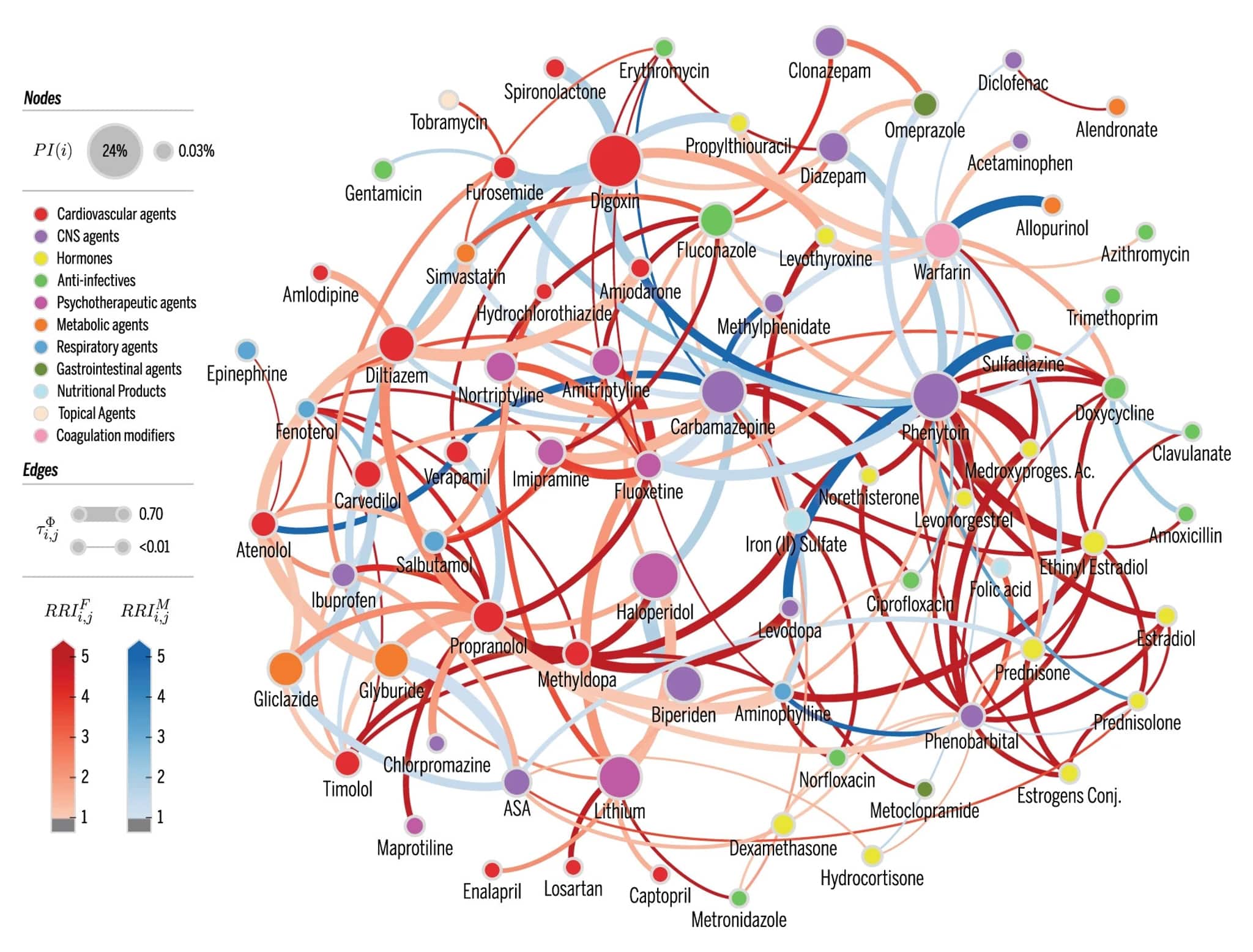
A total of 181 drug combinations prescribed against recommendations were uncovered. These medications, widely known to interact dangerously, were dispensed to 15,527 people among the study’s population, including 5,000 who got drug combinations known to cause major complications likely requiring medical attention.
“These results are surprising—shocking even—since it’s no secret these drugs aren’t supposed to be prescribed in combination,” says senior author of the study Luis Rocha, a professor in the Indiana University School of Informatics, Computing and Engineering. “We expected some elevated risk in the elderly since they use more medications, but not this high. The gender bias was completely unexpected.”
Drugs like ibuprofen and Prozac
According to the US Department of Health and Human Services, about one out of every three hospital visits annually are related to adverse drug effects, which include adverse drug reactions. Another analysis of adverse drug reaction in Ontario, Canada placed the cost of these incidents at nearly $12 million per year—or $1 per capita—for that province alone. In other countries, such as the US, the study’s authors estimate costs could run as much as seven times higher per capita.
The new analysis uses health records from Blumenau, a city in Brazil with a population of about 334,000. The researchers stumbled across gender- and age-based disparities in care during a general analysis of drug interactions among the city’s population in collaboration with researchers at the Regional University of Blumenau, which developed the city’s health record system. A PhD student in Rocha’s lab at the time of the study, Rion Brattig Correia, previously managed the lab that created the system.
The drugs identified as most commonly prescribed in dangerous combinations were standard medications—such as omeprazole, a common heartburn medication whose brand names include Prilosec; fluoxetine, a common antidepressant whose brand names include Prozac; and ibuprofen, a common analgesic—as well as some less common drugs, such as erythromycin, an anti-infectant.
The researchers were careful to control for other factors that might result in higher risk for dangerous drug combinations, such as older adults taking more prescription drugs, Rocha says. The study compares drugs actually prescribed to older patients against a random selection of drugs common among older adults, for example, to show that dangerous drug combinations actually occurred at a higher rate in real life compared to the random model.
Lack of options
Although the research did not explore the cause of these higher drug interaction risks, the lack of options for certain medications under Brazil’s public health system could play a role, Rocha adds. Women tend to be prescribed more antidepressants, for example, and more expensive options with fewer interactions are not available in the public health system. Similarly, older adults tend to use more medications to control cholesterol, another drug type with few public options found to occur often in dangerous combination.
“It might simply be that no other choice exists, so doctors feel that the treatment is worth the risks,” Rocha says. “Or some physicians may simply be unaware of the dangers.”
The researchers are hopeful the work might influence health policy in Brazil, Correia adds, including increasing publicly available drug choices for seniors and women. He plans to delve further into the results to learn the deeper causes of these biases against women and older adults.
“Physicians and other health care professions everywhere need to understand the role of gender and age toward the risk of dangerous drug interactions for their patients,” he says. “We expect these results will increase this awareness.”
Source: Indiana University