Researchers are developing a new recombinant flu vaccine that has the potential to compete with existing vaccines.
Recombinant protein vaccines, like the Novavax vaccine used to fight COVID-19, offer several advantages over conventional vaccines. They’re easy to precisely produce. They’re safe, and potentially more effective. And they could require smaller doses.
Because of these traits, there is much interest in developing recombinant influenza vaccines. To date, however, the Food and Drug Administration has approved only one such vaccine.
The researchers at the University at Buffalo hope to add to that number.
“Because of the variable nature of the viruses that cause influenza, current vaccines are not optimally effective among the overall population,” says Jonathan Lovell, professor in the biomedical engineering department at the University at Buffalo and senior coauthor of the study in the journal Cell Reports. “We believe our vaccine candidate has the potential to improve upon this by inducing stronger and broader immunity, and reducing the likelihood of illness and death.”
Conventional flu vaccines contain either deactivated microbes that cause influenza, or they are based on weakened forms of the disease. They are made using fertilized chicken eggs or, less commonly, through cell culture-based production.
The vaccine the research team is developing is based on a nanoliposome—a tiny spherical sac—that Lovell and colleagues created called cobalt-porphyrin-phospholipid, or CoPoP. The CoPoP platform enables immune response promoting proteins to be displayed on the surface of the nanoliposome, resulting in potent vaccine efficacy.
Alone, these nanoliposomes do not fight disease. But when combined with recombinant influenza proteins that can be generated based on genetic information from viruses, they enhance the immune system’s response to disease.
In the new study, the team attached to the nanoliposome a total of six proteins—three each from two different protein groups, hemagglutinins and neuraminidases. They also added two adjuvants (PHAD and QS21) to boost immune response.
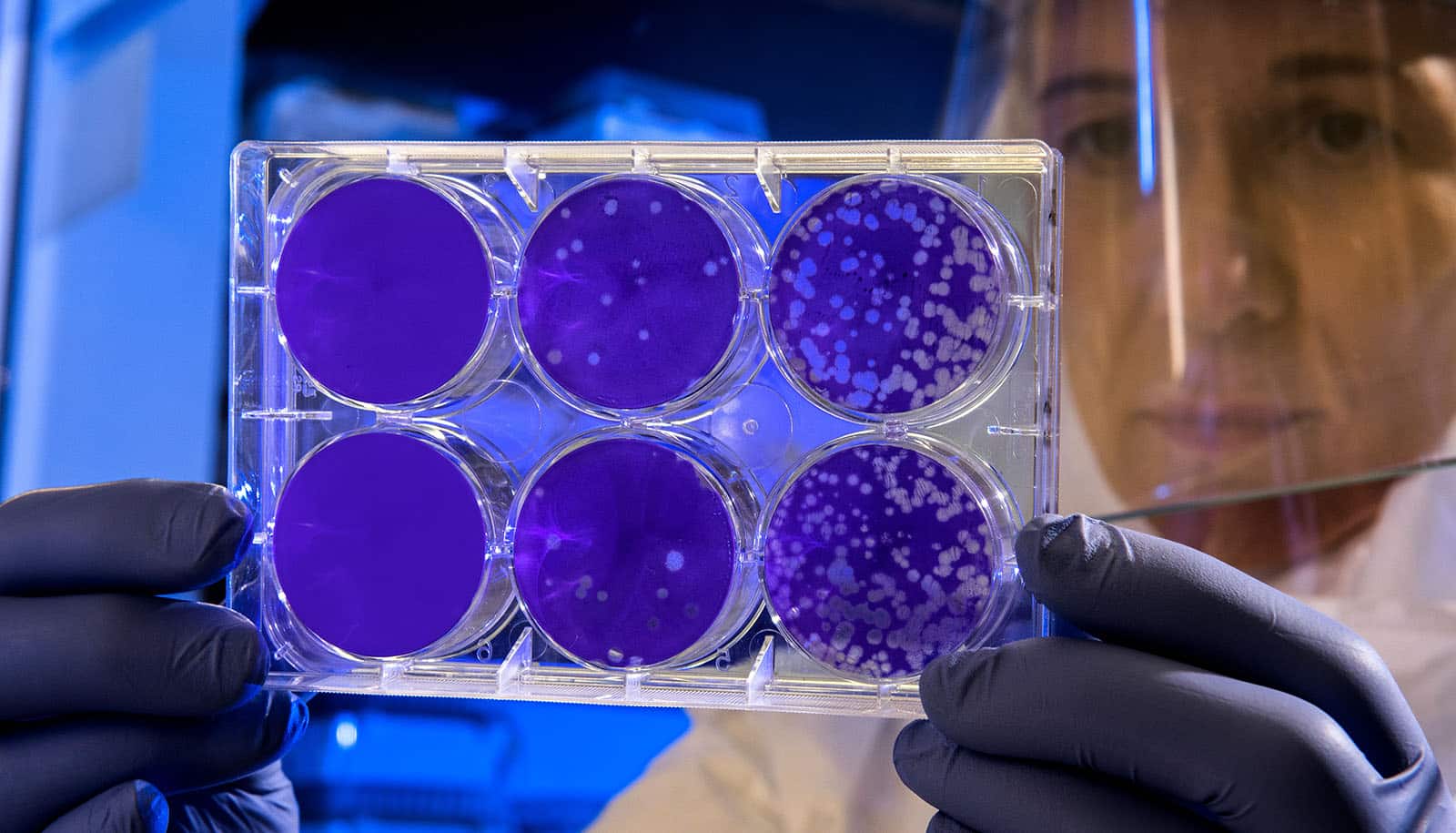
Researchers evaluated the resulting “hexaplex” nanoliposome in animal models with three common flu strains: H1N1, H3N2, and type B.
Even when administered in low doses, the hexaplex nanoliposome provided superior protection and survival from H1 and N1 when compared to Flublok, which is the sole licensed recombinant influenza vaccine in the US, and Fluaid, an egg-based vaccine. Tests showed comparable levels of protection against H3N2 and type B viruses.
The tests were performed via vaccination and through blood serum transfer from vaccinated mice into non-vaccinated mice.
“The combination of the two groups of proteins led to synergistic effects. In particular, the adjuvanted nanoliposomes excelled in the production of functional antibodies and the activation of T cells, which are critical to fighting off serious infection of the flu,” says lead author Zachary Sia, a PhD candidate in Lovell’s lab.
Bruce Davidson, a research associate professor of anesthesiology in the Jacobs School of Medicine and Biomedical Sciences, is a senior coauthor of the study.
He says “using not only hemagglutinin but also neuraminidase antigens to create vaccines is important because it translates into broader immunity and companies will be able to create more doses with less materials. That’s critical for not only the flu but also potential outbreaks like what we saw with COVID-19. There is still much work to be done in fully testing and validating this flu technology, but at this point these early results are quite promising.”
Additional coauthors are from the University at Buffalo and McGill University.
While not part of this study, the CoPoP vaccine platform underwent phase 2 and phase 3 clinical trials in South Korea and the Philippines as a COVID-19 vaccine candidate. This is a partnership between UB spinoff company POP Biotechnologies, cofounded by Lovell, and South Korean biotech company EuBiologics.
The researchers have filed patents with The Research Foundation for the State University of New York. Lovell and coauthor Wei-Chiao Huang, postdoctoral scholar in Lovell’s lab, are employed by POP Biotechnologies.
The National Institutes of Health funded the work.
Source: University at Buffalo