Probiotics, specifically lactobacillus, demonstrated a significant ability to delay a COVID infection and reduce symptoms among unvaccinated people who had been in contact with someone in their home diagnosed with COVID, researchers report in a new study.
The randomized, placebo-controlled study suggests that probiotics could be a relatively simple and inexpensive approach to treating people after a COVID exposure.
The finding could be a timely intervention as COVID-tracking data from the Centers for Disease Control and Prevention show hospital admissions and deaths on the rise in the US at the same time holiday celebrations will bring people together.
Additionally, fewer than 20% of the US population has received the 2023 updated COVID vaccine, according to the most recent CDC data.
“Prior to COVID, there was strong evidence that probiotics were protective against respiratory infections,” says Paul Wischmeyer, associate vice chair for clinical research in Duke University’s anesthesiology department and co-lead author of the study in the journal Clinical Nutrition.
“Once COVID hit, it was imperative to determine whether this simple, well-tolerated intervention could be useful. Our study provides encouraging evidence for the use of probiotics.”
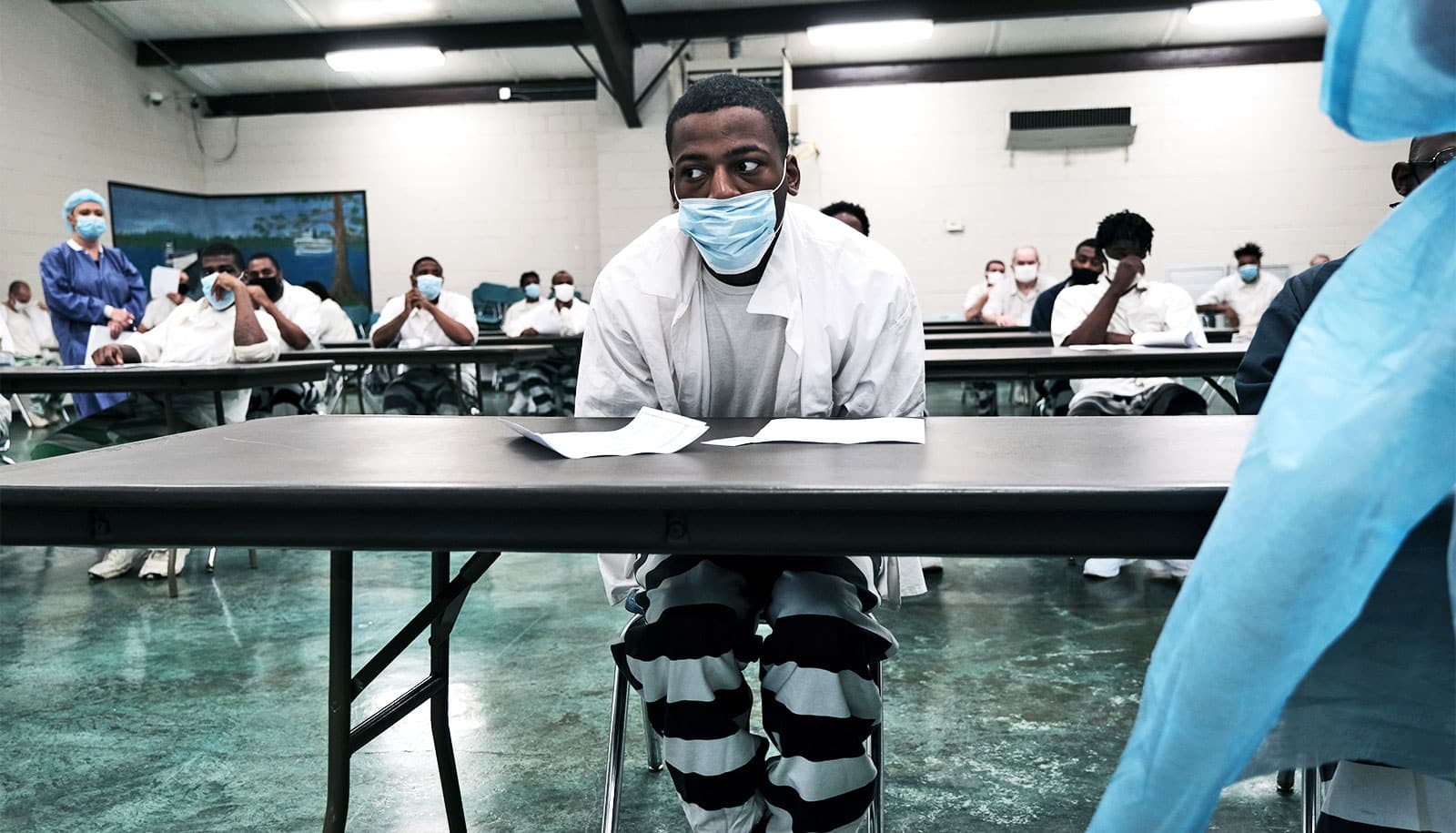
Wischmeyer and colleagues launched their investigation in March 2020, prior to widespread vaccine availability in the United States. Patients were enrolled if they were unvaccinated and had been exposed to someone with COVID, but had not yet exhibited symptoms.
The study enrolled 182 participants, with half randomly assigned to take a probiotic of lactobacillus and the other half randomized to take a placebo pill. Neither study participants nor administrators knew who was receiving the active therapy.
Wischmeyer says the study enrollment period was shortened because the pool of eligible participants declined as vaccines became more commonplace and infections began leveling off prior to the Delta wave.
Upon analysis, the researchers found that participants randomized to receive the probiotic were 60% less likely to develop COVID symptoms compared to those randomized to receive placebo—26.4% vs. 42.9%. The probiotic participants were also able to stave off infection longer compared to those receiving the dummy pill.
Although the probiotic group had a numerically lower incidence of COVID-19 diagnosis, the rate did not meet statistical significance (8.8% COVID diagnosis rate in probiotic vs. 15.4% COVID diagnosis rate in control group) because of the study size.
“We are actually not surprised by these findings,” Wischmeyer says. “There have been several studies that have demonstrated the strong efficacy of probiotics against respiratory infections, including a very large study among babies in India that was published in Nature in 2017.
“Other early studies have shown that probiotics may also enhance the effect of vaccines against other viral illnesses, such as influenza.”
Wischmeyer cited evidence that probiotics improve immune function in several ways, including increasing the population of regulatory T-cells, decreasing pro-inflammatory cytokines, increasing the lung’s protective barrier against infection, and modulating antiviral gene expression.
“While limited in sample size, our study lends credence to the notion that our symbiotic microbes can be valuable partners in the fight against COVID-19 and potentially other future pandemic diseases,” Wischmeyer says.
“This may be particularly relevant in under-resourced nations where vaccination rates have lagged and even in the US, where COVID boosters are not widely accessed.”
The Duke Microbiome Center and private philanthropic donations supported the work. DSM/iHealth donated the probiotic and placebo pills for the trial, but had no role in the study’s design, conduct, analysis, or writing.
Source: Duke University