Placental examination resulted in the accurate pathologic determination of more than 90% of previously unexplained pregnancy losses, report researchers.
There are approximately 5 million pregnancies per year in the United States, with 1 million ending in miscarriage (a loss occurring prior to 20 weeks of gestation) and over 20,000 ending in stillbirth at or beyond 20 weeks of gestation. As many as 50% of these losses are categorized as “unspecified.”
Patients who suffer such pregnancy outcomes are often told that their loss is unexplained and that they should simply try again, contributing to patients’ feeling of responsibility for the loss, says senior author Harvey Kliman, a research scientist in the department of obstetrics, gynecology, and reproductive sciences at Yale School of Medicine.
“To have a pregnancy loss is a tragedy. To be told there is no explanation adds tremendous pain for these loss families,” says Kliman, who is also director of the Reproductive and Placental Research Unit. “Our goal was to expand the current classification systems to decrease the number of cases that remained unspecified.”
For the study, Kliman worked with Beatrix Thompson, currently a medical student at Harvard University, and Parker Holzer, a former graduate student in Yale’s department of statistics and data science, to develop an expanded classification system for pregnancy losses based on pathologic examination of loss placentas. The findings appear in the journal Reproductive Sciences.
The team started with a series of 1,527 single-child pregnancies that ended in a loss that were sent to Kliman’s consult service for evaluation. After excluding cases without adequate material for examination, 1,256 placentas from 922 patients were examined. Of these, 70% were miscarriages and 30% were stillbirths.
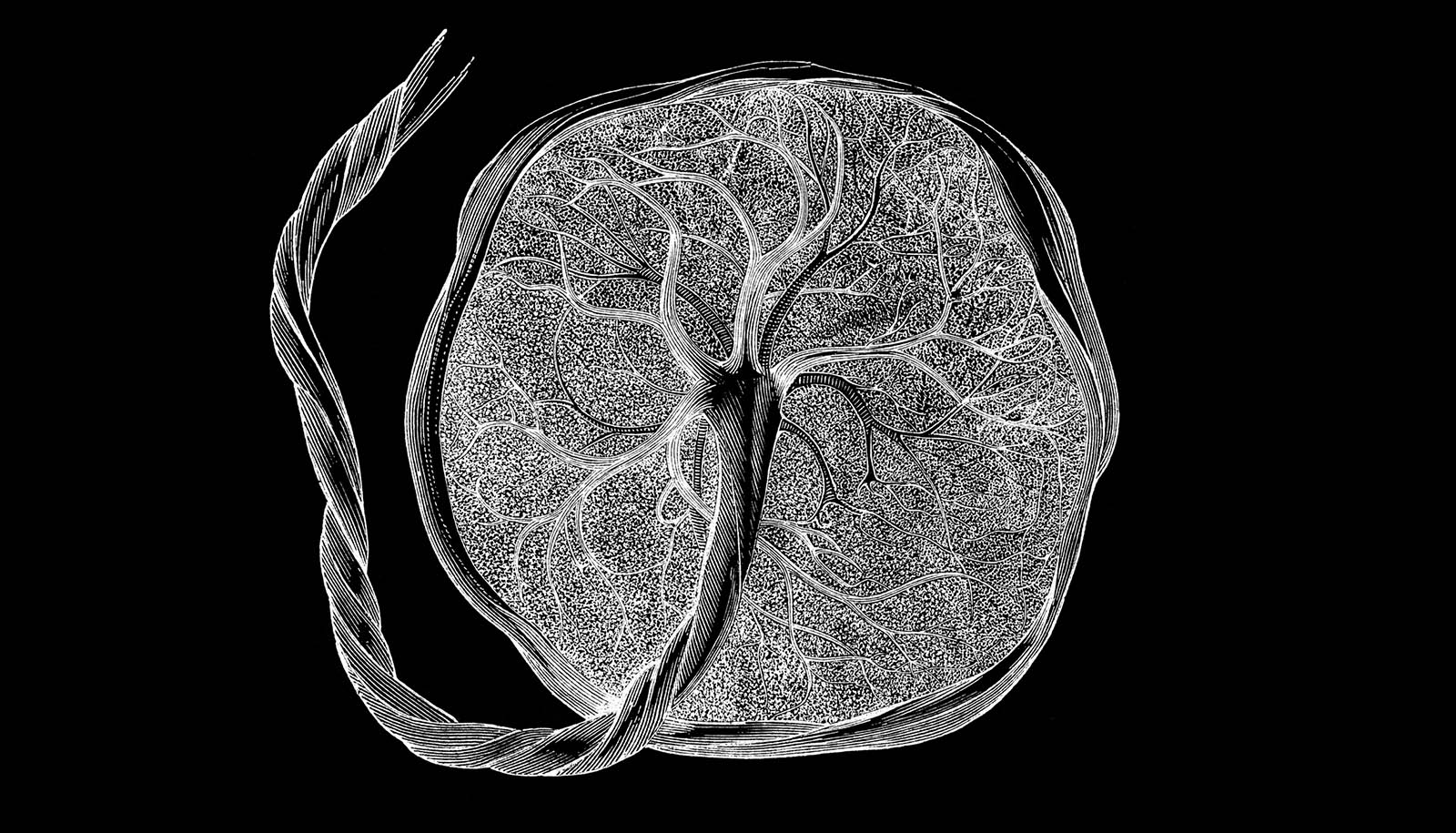
By adding the explicit categories of “placenta with abnormal development” (dysmorphic placentas) and “small placenta” (a placenta less than the 10th percentile for gestational age) to the existing categories of cord accident, abruption, thrombotic, and infection, for example, the authors were able to determine the pathologic diagnoses for 91.6% of the pregnancies, including 88.5% of the miscarriages and 98.7% of the stillbirths.
The most common pathologic feature observed in unexplained miscarriages were dysmorphic placentas (86.2%), a marker associated with genetic abnormalities. The most common pathologic feature observed in unexplained stillbirths was a small placenta (33.9%).
“This work suggests that the over 7,000 small placentas per year associated with stillbirths could have been detected in utero—flagging those pregnancies as high risk prior to the loss,” says Kliman. “Likewise, the identification of dysmorphic placentas may be one way to potentially identify genetic abnormalities in the almost 1 million miscarriages that occur in our country every year.”
He adds, “Having a concrete explanation for a pregnancy loss helps the family understand that their loss was not their fault, allows them to start the healing process, and, when possible, prevent similar losses—especially stillbirths—from occurring in the future.”
When asked what the most effective way might be to prevent stillbirths, Kliman responds, “Measure the placenta!”
Source: Yale University