Two distinct neurodevelopmental abnormalities that arise just weeks after the start of brain development have been associated with the emergence of autism spectrum disorder, according to a new study.
And, researchers say, the specific abnormalities seem to be dictated by the size of the child’s brain, a finding that could help doctors and researchers to diagnosis and treat autism in the future.
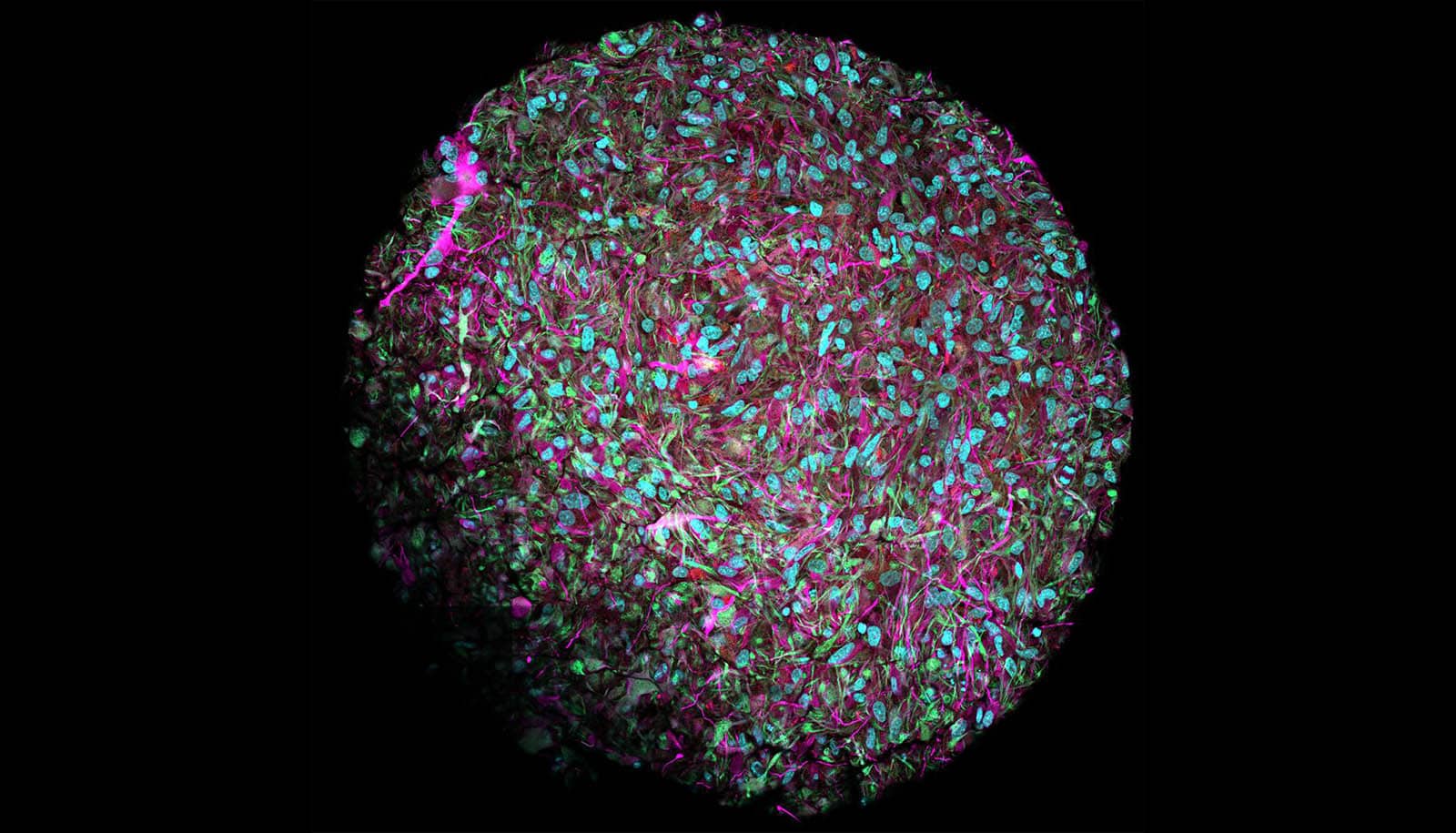
The findings, from the study in which researchers developed brain organoids from the stem cells of boys diagnosed with the disorder, appear in the journal Nature Neuroscience.
“It’s amazing that children with the same symptoms end up with two distinct forms of altered neural networks,” says Flora Vaccarino, a professor in the Child Study Center at Yale School of Medicine and co-senior author of the paper.
Using stem cells collected from 13 boys diagnosed with autism—including eight boys with macrocephaly, a condition in which the head is enlarged—the team created brain organoids (small, three-dimensional replicas of the developing brain) in a lab dish that mimic neuronal growth in the fetus. They then compared brain development of these affected children with that of their fathers. (Patients were recruited from clinician colleagues at the Yale Child Study Center, which conducts research, service, and training to improve understanding of health issues facing children and their families.)
About 20% of autism cases involve individuals with macrocephaly, a condition in which a child’s head size is in the 90th percentile or greater at birth. Among autism cases, these tend to be more severe.
Intriguingly, the researchers found that children with autism and macrocephaly exhibited excessive growth of excitatory neurons compared with their fathers while organoids of other children with autism showed a deficit of the same type of neurons.
The ability to track the growth of specific types of neurons could help doctors diagnose autism, symptoms of which generally appear 18 to 24 months after birth, the authors say.
The findings may also help identify autism cases that might benefit from existing drugs designed to ameliorate symptoms of disorders marked by excessive excitatory neuron activity, such as epilepsy, Vaccarino says. Autism patients with macrocephaly might benefit from such drugs while those without enlarged brains may not, she says.
Creating biobanks of patient-derived stem cells could be essential to tailor therapeutics to specific individuals, or personalized medicine.
Coauthors of the paper are from Yale and the Mayo Clinic.
Source: Yale University