A new upgraded model shows how the body’s immune response can make tumor cells more resistant to chemotherapy.
Tumor cells won’t show their true selves in a Petri dish, isolated from other cells. To find out how they really behave, researchers developed the new model that houses osteosarcoma cells beside immune cells known as macrophages inside a three-dimensional structure engineered to mimic bone.
The study, published in Biomaterials, sheds light on why some cancer drugs that appear to be good candidates in the lab do not perform as well as expected in actual patients. It underscores weaknesses in traditional tumor modeling and points the way toward more effective cancer therapies.
“Existing tumor models used to test drug performance do not mimic the actual environment in the human body closely enough,” says Antonios Mikos, a professor of bioengineering and chemical and biomolecular engineering at Rice University.
“We are trying to create an environment for the experiment that is closer to what is happening in the organism of actual patients. Having such an environment will allow us to test multiple drugs in a time- and cost-effective way.”
Mikos’ lab had shown in previous work that cancer cells are sensitive to the mechanical properties of their substrate.
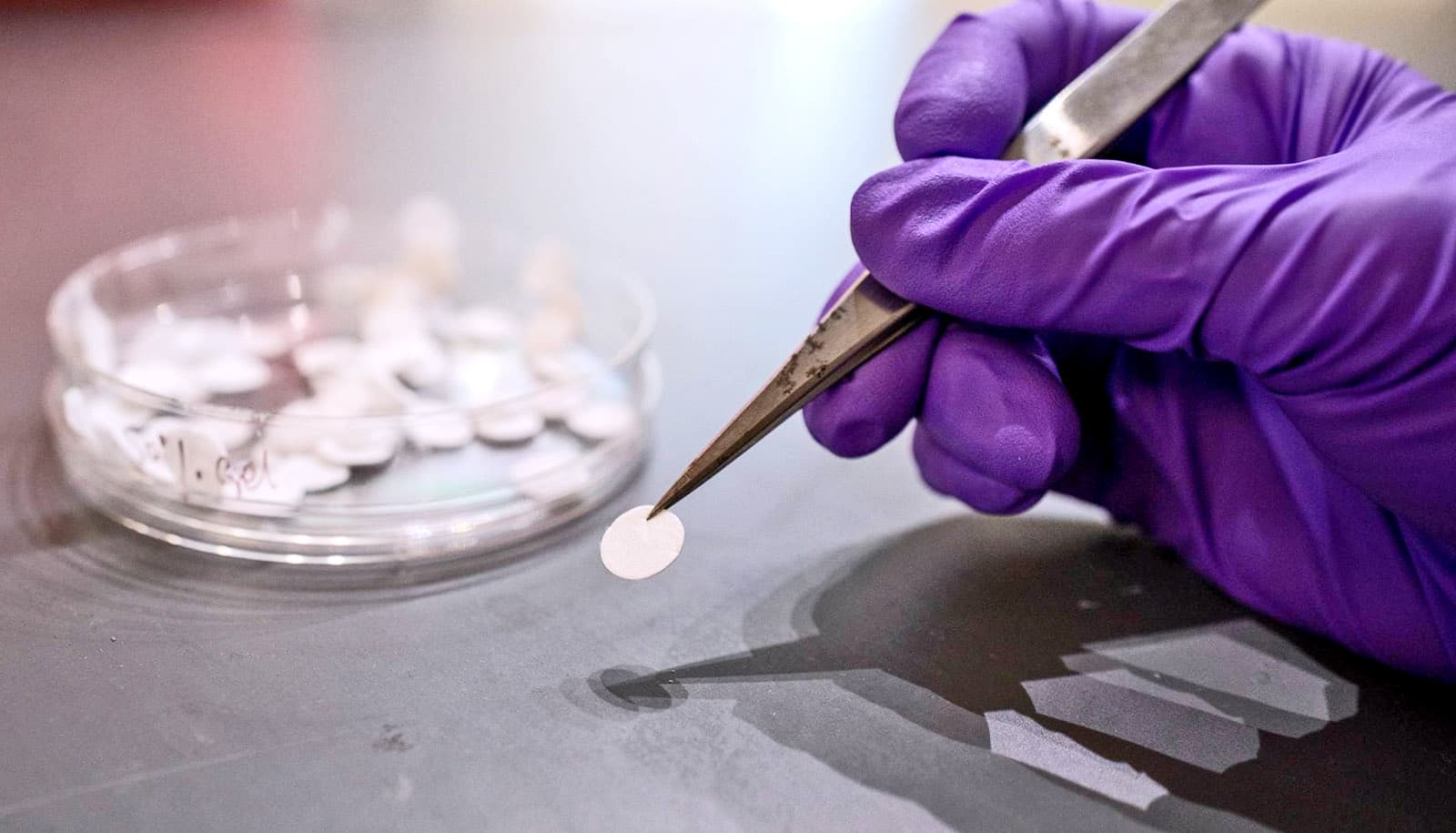
“Typically, cells would be grown on a flat surface, like in a Petri dish,” says lead author Letitia Chim, who recently earned a doctorate at Rice. “If you use a microscope to look at the disc-shaped scaffolds we developed, you can see that they are made up of these fiber structures on the scale of what cells would recognize. The cells can sense that this substrate is three-dimensional instead of flat—closer to what bone structure is like.”
The scaffolds are made from two different materials: a very stiff synthetic polymer and gelatin. By changing the ratio of the materials, researchers can control the overall stiffness of the fibers.
“What is new here and very revealing is that we added the next level of complexity—the immune cells that are part of the tumor microenvironment—and looked at how the combination of the mechanical responsiveness of the substrate and the presence of other cells factors into tumor development and behavior,” Mikos says.
“In a tumor, you don’t only have the cancer cells, you have other cells that are sending out signals that can affect how the cancer cells will respond to treatment,” Chim says.
Researchers found that increased inflammation caused by macrophages reduced the effectiveness of doxorubicin, one of the chemotherapeutic agents used to treat osteosarcoma, which is the most common form of bone cancer.
“We were interested in tumor-associated macrophages because they can make up to 50% of the tumor,” Chim says. “Tumors have sometimes been described as wounds that never heal, and that’s partly due to the macrophages sending out wound-healing signals. In normal tissue that works well, but it can also benefit the tumor.”
Preclinical models that mimic tumors more accurately can help researchers identify which therapies are most effective in a given context.
“This is going to be useful in order to design therapeutics that target not only the cancer cells but also the immune cells, or that trigger the immune cells to essentially change their function,” Mikos says.
“A major objective of our research is to develop personalized testing systems or platforms where the characteristics of the patient’s tumor are used to find a therapeutic model that works best for them,” Chim says. “I would say that’s the personalized medicine vision of the future: being able to answer the question, are there particular targeted treatments that work well for this patient?
“Osteosarcoma is a rare disease that often gets overlooked. It’s also a really complicated disease that shows up differently in every single patient. This is another reason why it would ultimately be great if we can develop a personalized medicine approach for treating osteosarcoma.”
“The tumor microenvironment clearly plays an important role in how disease progression and treatment unfold,” Mikos says. “That is why we strive to develop an optimal level of complexity that captures the bigger picture of what actually happens inside a live organism.”
The National Institutes of Health funded the research.
Source: Rice University