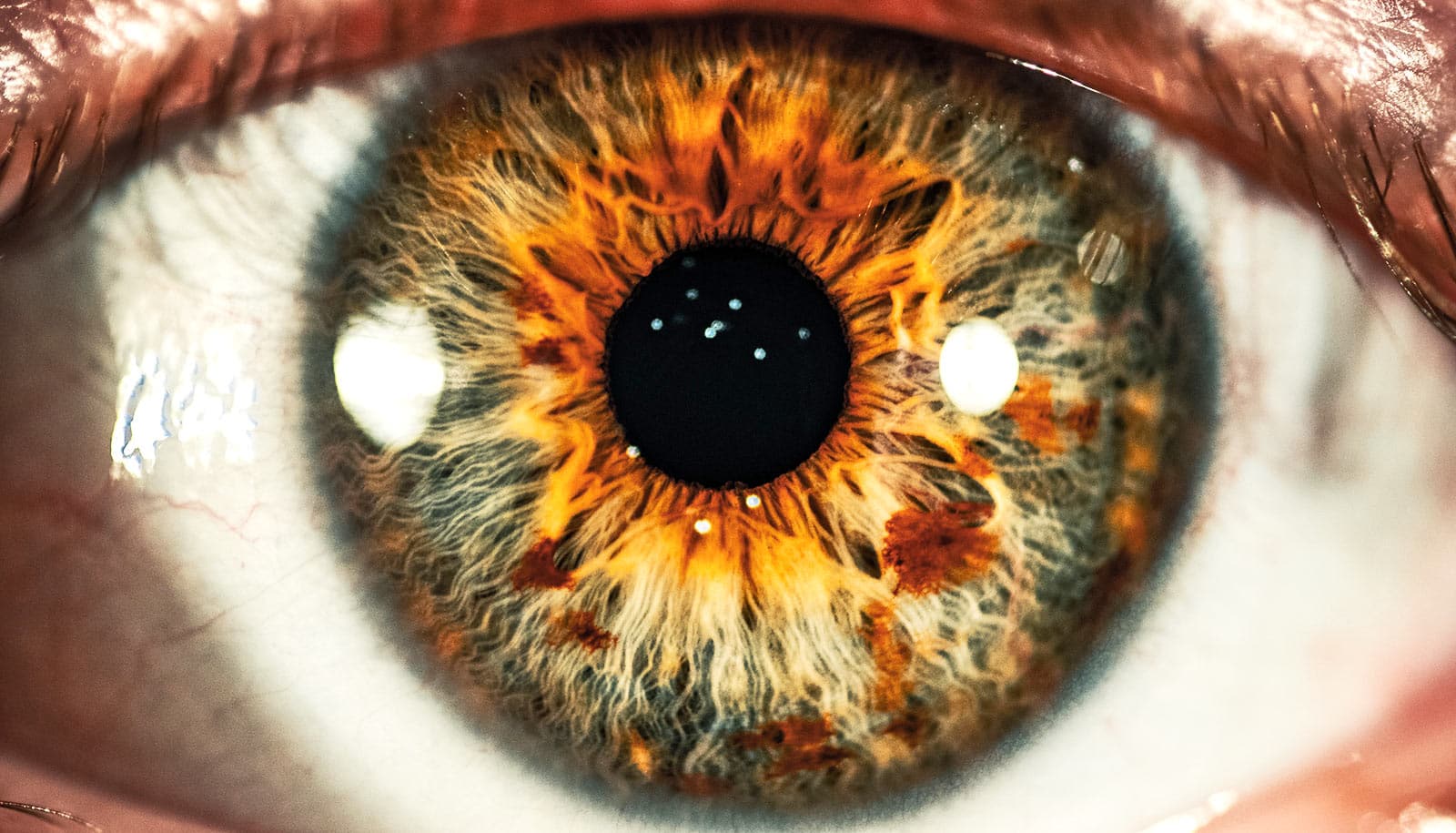
A new study with mice finds that proteins made by stem cells that regenerate the cornea may be new targets for treating and preventing injuries.
People with a condition known as dry eye disease are more likely than those with healthy eyes to suffer injuries to their corneas.
Dry eye disease occurs when the eye can’t provide adequate lubrication with natural tears. People with the common disorder use various types of drops to replace missing natural tears and keep the eyes lubricated, but when eyes are dry, the cornea is more susceptible to injury.
“We have drugs, but they only work well in about 10% to 15% of patients,” says senior investigator Rajendra S. Apte, professor in the department of ophthalmology and visual sciences at Washington University in St. Louis.
“In this study involving genes that are key to eye health, we identified potential targets for treatment that appear different in dry eyes than in healthy eyes.
“Tens of millions of people around the world—with an estimated 15 million in the United States alone—endure eye pain and blurred vision as a result of complications and injury associated with dry eye disease, and by targeting these proteins, we may be able to more successfully treat or even prevent those injuries.”
For the study in the Proceedings of the National Academy of Sciences, the researchers analyzed genes expressed by the cornea in several mouse models—not only of dry eye disease, but also of diabetes and other conditions. They found that in mice with dry eye disease, the cornea activated expression of the gene SPARC. They also found that higher levels of SPARC protein were associated with better healing.
“We conducted single-cell RNA sequencing to identify genes important to maintaining the health of the cornea, and we believe that a few of them, particularly SPARC, may provide potential therapeutic targets for treating dry eye disease and corneal injury,” says first author Joseph B. Lin, an MD/PhD student in Apte’s lab.
“These stem cells are important and resilient and a key reason corneal transplantation works so well,” Apte explains. “If the proteins we’ve identified don’t pan out as therapies to activate these cells in people with dry eye syndrome, we may even be able to transplant engineered limbal stem cells to prevent corneal injury in patients with dry eyes.”
The National Eye Institute, the National Institute of Diabetes and Digestive and Kidney Diseases, and the National Institute of General Medical Sciences of the National Institutes of Health supported the work. Additional funding came from the Jeffrey T. Fort Innovation Fund, a Centene Corp. contract for the Washington University-Centene ARCH Personalized Medicine Initiative, and Research to Prevent Blindness.