Researchers are working on the development of a treatment that targets a molecule that acts as a central executioner in the death of axons.
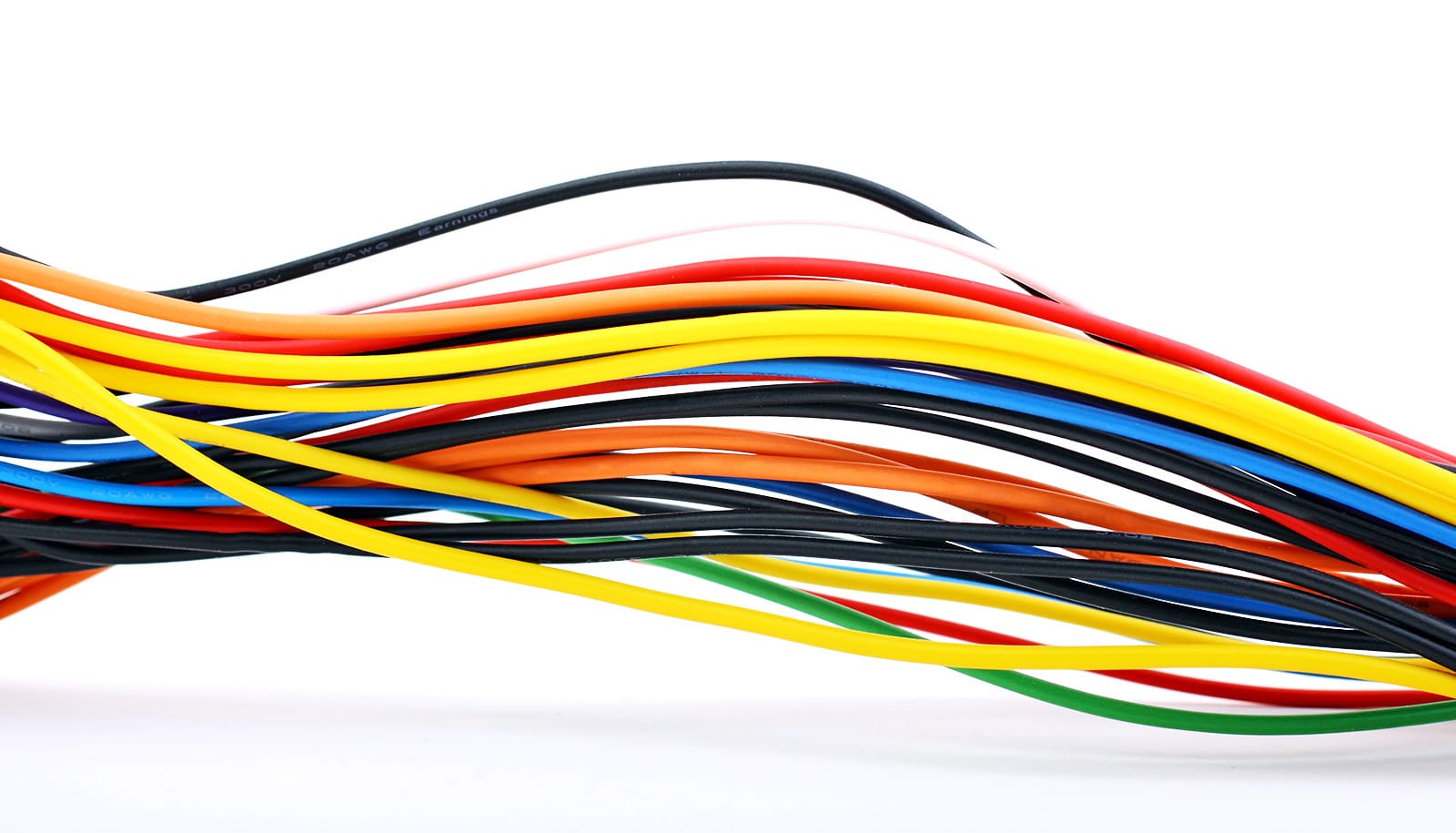
Axons are the wiring of the nervous system.
Blocking this molecular executioner prevents axon loss, which has been implicated in many neurodegenerative diseases, including peripheral neuropathies, Parkinson’s disease, glaucoma, and amyotrophic lateral sclerosis (ALS).
Two studies, both published in the Journal of Clinical Investigation (study one, study two), reveal surprising details about how the molecule—called SARM1— triggers axon death that underlies the development of neurodegenerative diseases. The research also points to new therapeutic approaches for diseases defined by axon loss.
“We desperately need treatments for neurodegenerative diseases,” says co-senior author Jeffrey Milbrandt, professor and head of the genetics department at Washington University in St. Louis.
“With the evidence of SARM1’s central role in these diseases, we’re very interested in finding ways to block this molecule—whether with small molecule inhibitors or gene therapy techniques. Our latest research suggests we also may be able to interfere with its ability to drive damaging neuroinflammation. We’re hopeful this work will lead to effective new therapies across a range of neurodegenerative and neuroinflammatory diseases.”
In 2017, Milbrandt and co-senior author Aaron DiAntonio, professor of developmental biology, discovered that SARM1 is an enzyme that can promote neurodegeneration.
In healthy neurons, SARM1 is always switched off. But after injury or due to disease, SARM1 becomes active. Activated SARM1 is an arsonist—burning so much cellular energy that the axons can’t survive. This energy crisis triggers axons to disintegrate.
To understand more about SARM1’s role in triggering axon destruction, the researchers studied a mysterious and extremely rare progressive neuropathy syndrome—so rare, it lacks a name. This rare disease turned out to be a good model for understanding the role of the immune system in neuroinflammatory conditions generally.
Sequencing patient genomes, the researchers found that the axon loss was caused by genetic errors in the gene NMNAT2, whose normal function keeps SARM1 turned off. Due to these genetic errors, SARM1 is constantly activated, which triggers axon destruction. The researchers used the CRISPR gene-editing technique to reproduce these mutations in mice. Like people with the syndrome, these mice survived to adulthood but had worsening motor dysfunction, loss of peripheral axons, and, importantly, an infiltration of immune cells called macrophages.
The researchers were surprised to find that reducing the number of macrophages reversed the axon loss and disease symptoms in the mice. The study suggests that SARM1 not only contributes directly to axon loss but also plays a role in driving neuroinflammation that only serves to compound the problems.
The findings also suggest that some neurodegenerative conditions could be treated with immune modulating drugs that block macrophages or other inflammatory immune cells.
In the second paper, the researchers investigated the possible role of SARM1 in Charcot-Marie-Tooth disease type 2a, a common form of inherited peripheral neuropathy and a good model to study axon loss generally.
Patients with this disease have progressive loss of motor and sensory axons and develop difficulty walking, muscle weakness, and tingling or burning sensations in the hands and feet. The disease is caused by a mutation in an important protein in mitochondria, the energy factories of cells. The mutation, in a protein called mitofusin2, impairs the normal function of mitochondria. Much research has focused on the abnormal mitochondria, assuming they must be the root of the problem in this disease.
Surprisingly, the researchers found that deleting SARM1 in a rodent model of Charcot-Marie-Tooth disease type 2a stopped most of the problems the animals exhibited—independent of the diseased mitochondria.
Eliminating SARM1 blocked or slowed axon death, muscle atrophy, mitochondrial abnormalities, and problems with neuromuscular junctions, where the neurons interface with muscle. Even with the mutant mitofusin2 protein present, deleting SARM1 protected the mitochondria from further degradation and dysfunction.
“When we block SARM1, we not only protect the axons, we get much healthier mitochondria,” DiAntonio says. “This was a complete surprise, but we are hopeful it could be relevant in many neurodegenerative diseases where mitochondrial damage is central, such as Parkinson’s disease, as many neurodegenerative diseases have a component of mitochondrial dysfunction.”
Milbrandt and DiAntonio are co-founders, scientific advisory board members, and shareholders of Disarm Therapeutics, a wholly owned subsidiary of Eli Lilly and Company. Disarm Therapeutics and Eli Lilly are developing SARM1-targeted therapies for neurodegenerative diseases.
The National Institutes of Health, the Needleman Center for Neurometabolism and Axonal Therapeutics, and Washington University Institute of Clinical and Translational Sciences, supported the work.