A synthetic antibody can act as a decoy to intercept and neutralize the coronavirus that leads to COVID-19 before it can cause infection, according to new research with mice.
Scientists working to develop drugs against COVID-19 are focused on interrupting its interaction with ACE2, an enzyme the spike protein on the surface of the coronavirus latches onto, like a key, to enter and infect healthy cells.
“…we think it would work as an injection either once every two weeks or maybe even once a month.”
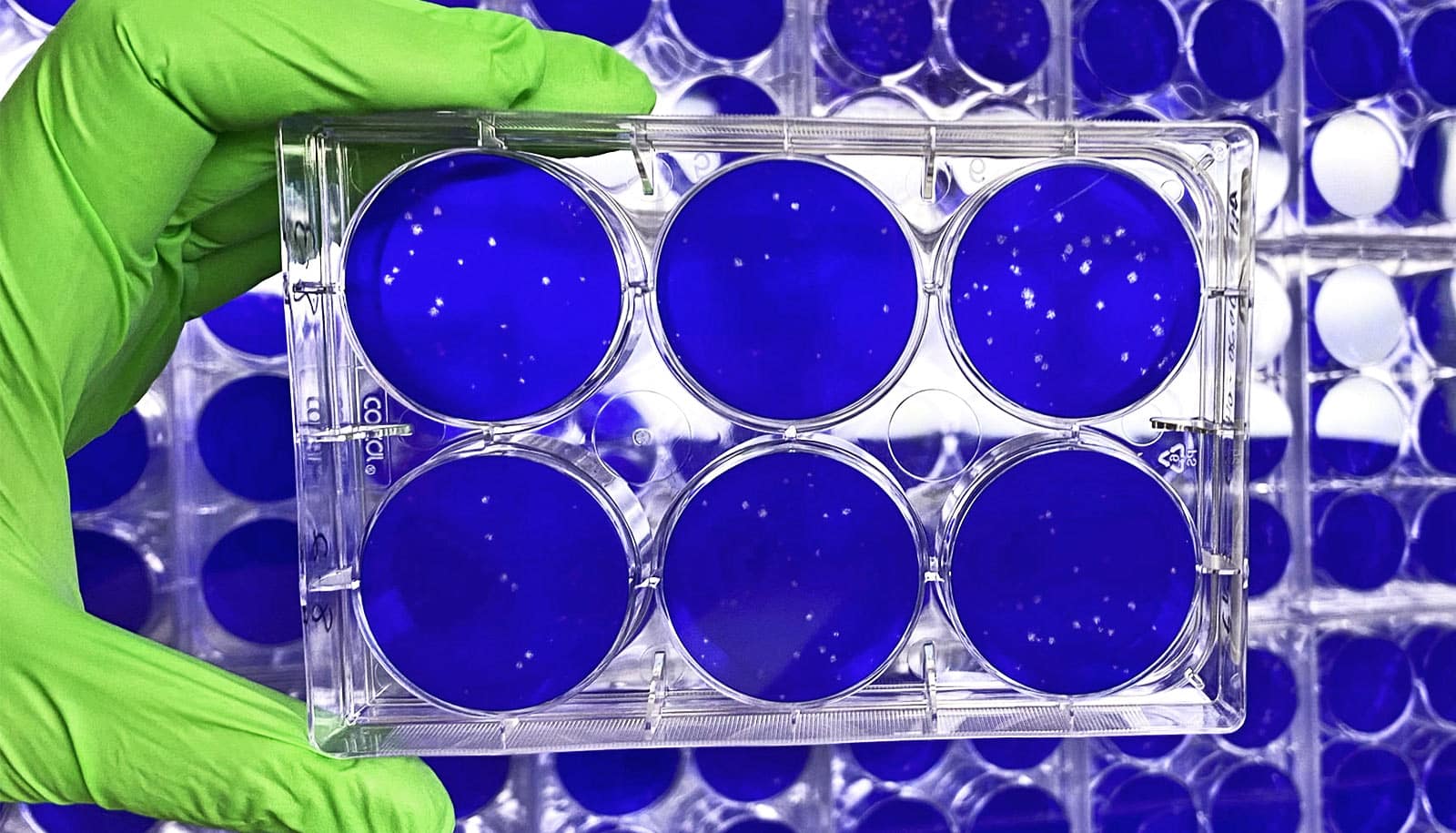
The synthetic protein, MDR504, effectively blocked the SARS-COV-2 virus from attaching to ACE2 in cell cultures, according to the early research.
“Unlike other agents in development against the virus, this protein is engineered to go to the lungs to neutralize the virus before it can infect lung cells,” says lead author Jay Kolls, chair in internal medicine at Tulane University’s School of Medicine.
Researchers fused a modified version of the ACE2 protein to the end of an antibody to create MDR504.
In the study using a mouse model, they showed that the drug circulated in blood and lung tissue at levels likely to be effective against the virus.
In addition to a treatment, the drug could be used as a pre- or post-exposure therapy for healthcare workers, first responders and vulnerable populations at highest risk. It also could be used to prevent infection in patients with underlying illness who couldn’t receive a vaccine.
Preliminary research shows that the drug could work at relatively low doses, Kolls says.
“Based on our data, we think it would work as an injection either once every two weeks or maybe even once a month,” Kolls says.
The concept behind the compound is similar to Enbrel, which is used to treat arthritis and other autoimmune disorders.
The research appears on bioRxiv, a preprint server for scholarly articles in the health sciences that are not yet peer-reviewed.
Tulane and Kolls are working with MDR Logix, LLC, a New Orleans based biotech company, to commercialize the discovery to begin a phase I clinical trial.
Source: Tulane University