Fecal transplants with only viruses show promise for treating obesity and type 2 diabetes.
Currently, fecal transplants are an option for treating certain types of antibiotic-resistant diarrhea, and have been an attempted treatment for inflammatory bowel disease.
In the study, obese mice with unhealthy lifestyles gained significantly less weight and avoided type 2 diabetes when they received viruses transplanted from the stool of lean mice.
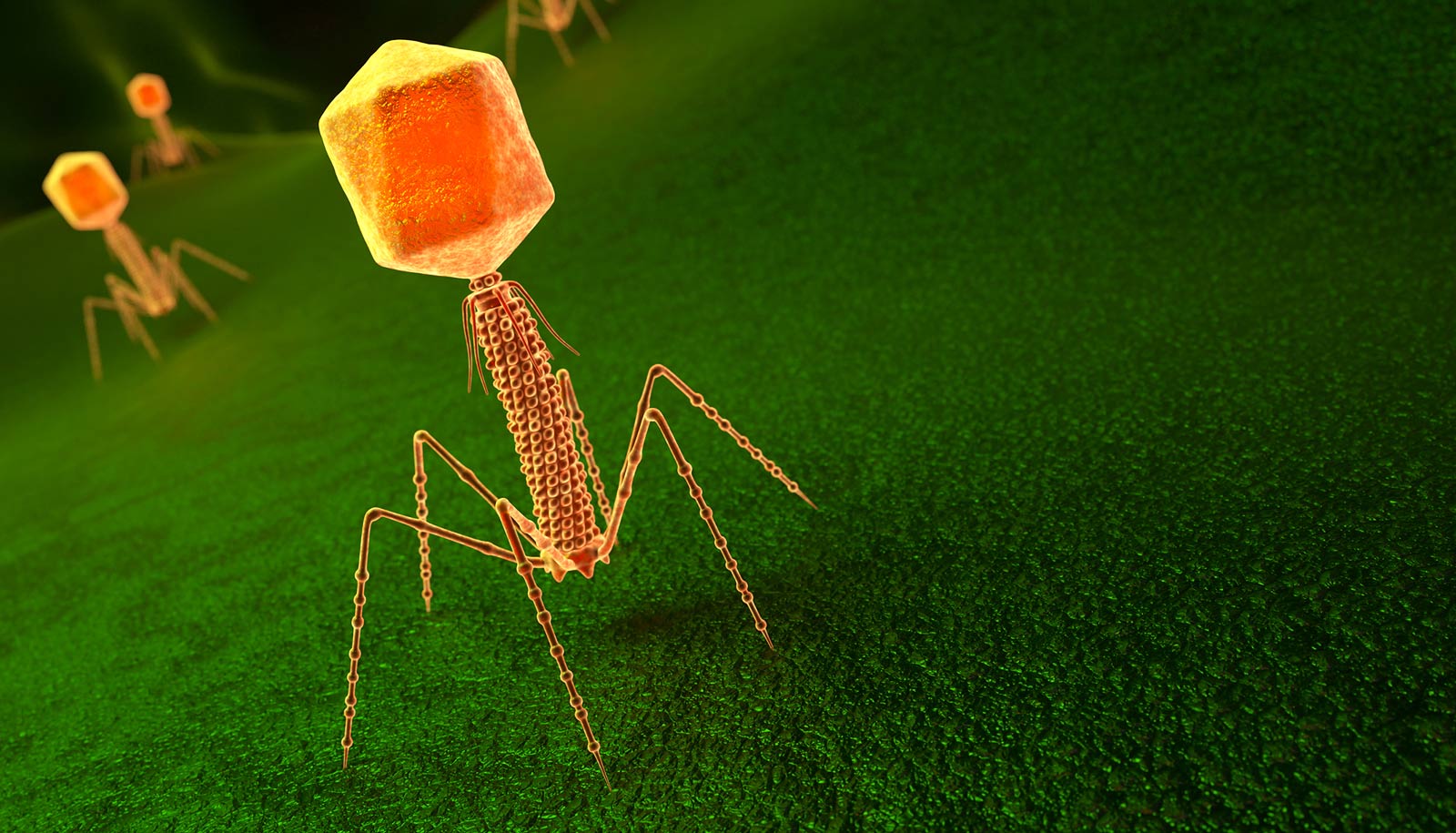
In recent years, fecal transplants from healthy donors to sick patients have become a popular way of treating a serious type of diarrhea caused by the bacterium Clostridioides difficile in humans. Recent trials in mice suggest that a similar treatment, which transplants only the viruses in stool, may help people suffering from obesity and type 2 diabetes. The majority of virus particles transmitted are bacteriophages—viruses that specifically attack bacteria and not humans.
“When we transmit virus particles from the feces of lean mice to obese ones, the obese mice put on significantly less weight compared to those that do not receive transplanted feces,” says senior author of the study Dennis Sandris Nielsen, professor in the University of Copenhagen’s food science department.
The method also seems to protect the mice against developing glucose intolerance (a hallmark of type 2 diabetes), a disease that inhibits the body from properly absorbing sugar. The experiments demonstrated that the obese mice that received an intestinal virus transplant from lean mice reacted to a shot of glucose no differently than the lean ones.
“In the obese mice on high fat diet that didn’t receive the virus transplant, we observed decreased glucose tolerance, which is a precursor of diabetes. Thus, we have influenced the gut microbiome in such a way that the mice with unhealthy lifestyles do not develop some of the common diseases triggered by poor diet,” explains PhD student Torben Sølbeck Rasmussen, first author of the study.
He emphasizes that the method is not a stand-alone solution and that a change in diet needs to accompany it. Furthermore, the treatment will probably not be targeted at general obesity, but more towards the most serious cases.
It is understood that obesity and type 2 diabetes are linked to imbalances in the gastrointestinal microbiome, also known as gut flora. In recent years, research has shown that the composition of viruses in the gut plays a crucial role in the balance of this microbiome.
“Here, we have a means of recuperating balance by shooting missing virus particles back into the system,” says Nielsen.
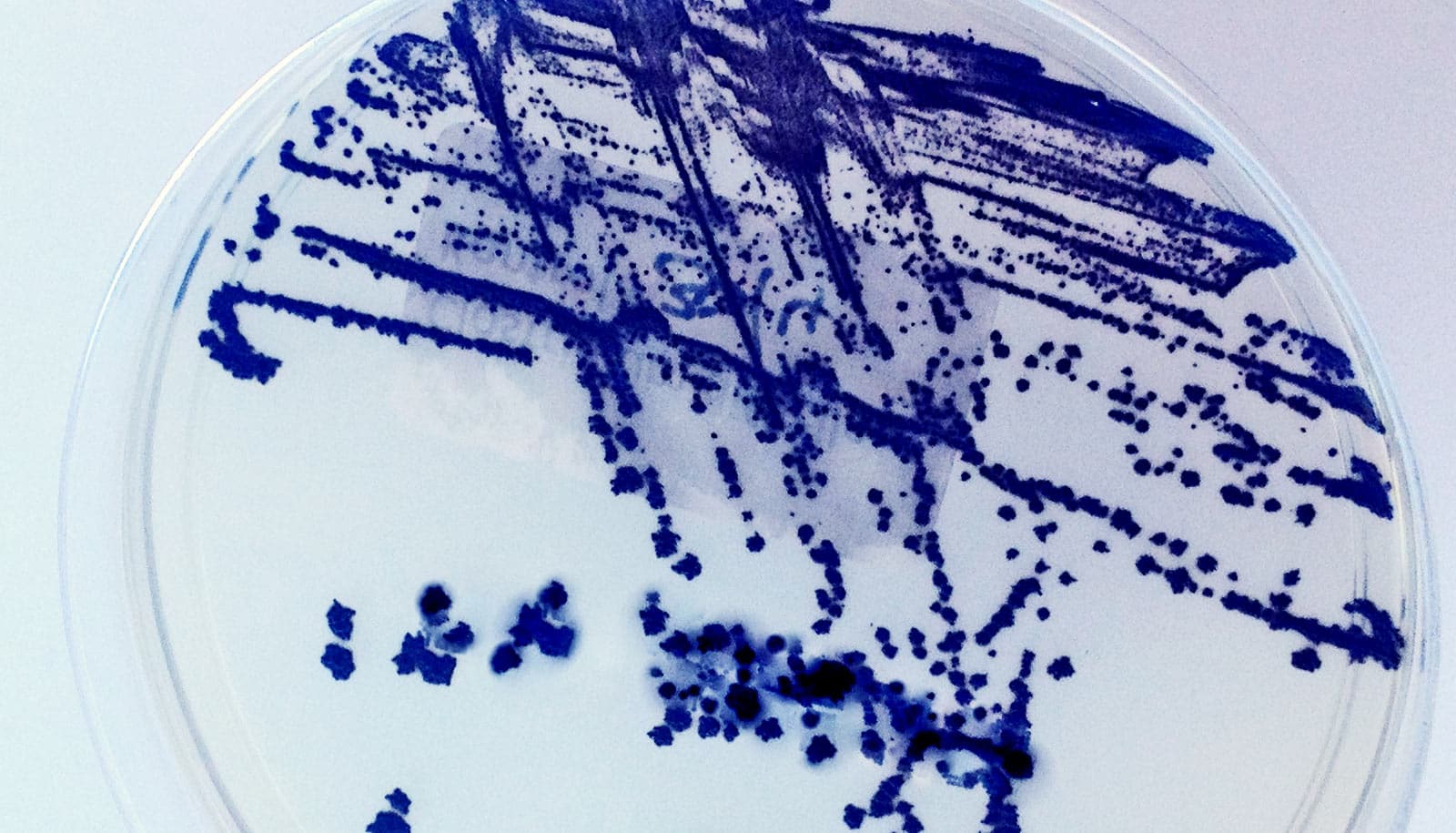
The researchers extracted feces from mice fed a standard low-fat diet over a period of time. The stool was then filtered so that all live bacteria were sorted out, while the virus particles—mainly bacteriophages—were concentrated. The viruses were transplanted via a tube into the mice that had been on high-fat diets for six weeks. The mice continued the fatty diet for another six weeks. Then, the researchers examined the mice after a glucose test and measured for weight gain.
The study addresses one of the current problems with fecal transplants. Today, stool is transplanted in an unfiltered form, in the belief that it is the gut bacteria which are most effective. However, in rare cases, the method produces side effects when the procedure inadvertently transplants diseases via the transplanted stool bacteria. A patient in the United States died from just such an occurrence last year.
“Our study demonstrates that there is an effect after the live bacteria have been filtered from stool. Therefore, primarily virus particles are transmitted. This makes the method safer,” says Nielsen.
He expects that it will be a number of years before the method can be broadly deployed. More experiments are needed, and obviously, human trials as well.
“Mice are the first step. But because the findings suggest that it will work in humans, that is the next. Our hope is that, in the long term, a well-defined cocktail of bacteriophages can be developed that has a minimal risk of side effects,” concludes Nielsen.
Additional researchers from the University of Copenhagen and Imperial College London contributed to the work, which appears in the journal Gut.
The Danish Council for Independent Research supported the work.
Source: University of Copenhagen