Artificial intelligence can help doctors and patients with meningiomas make better treatment decisions, according to a new study.
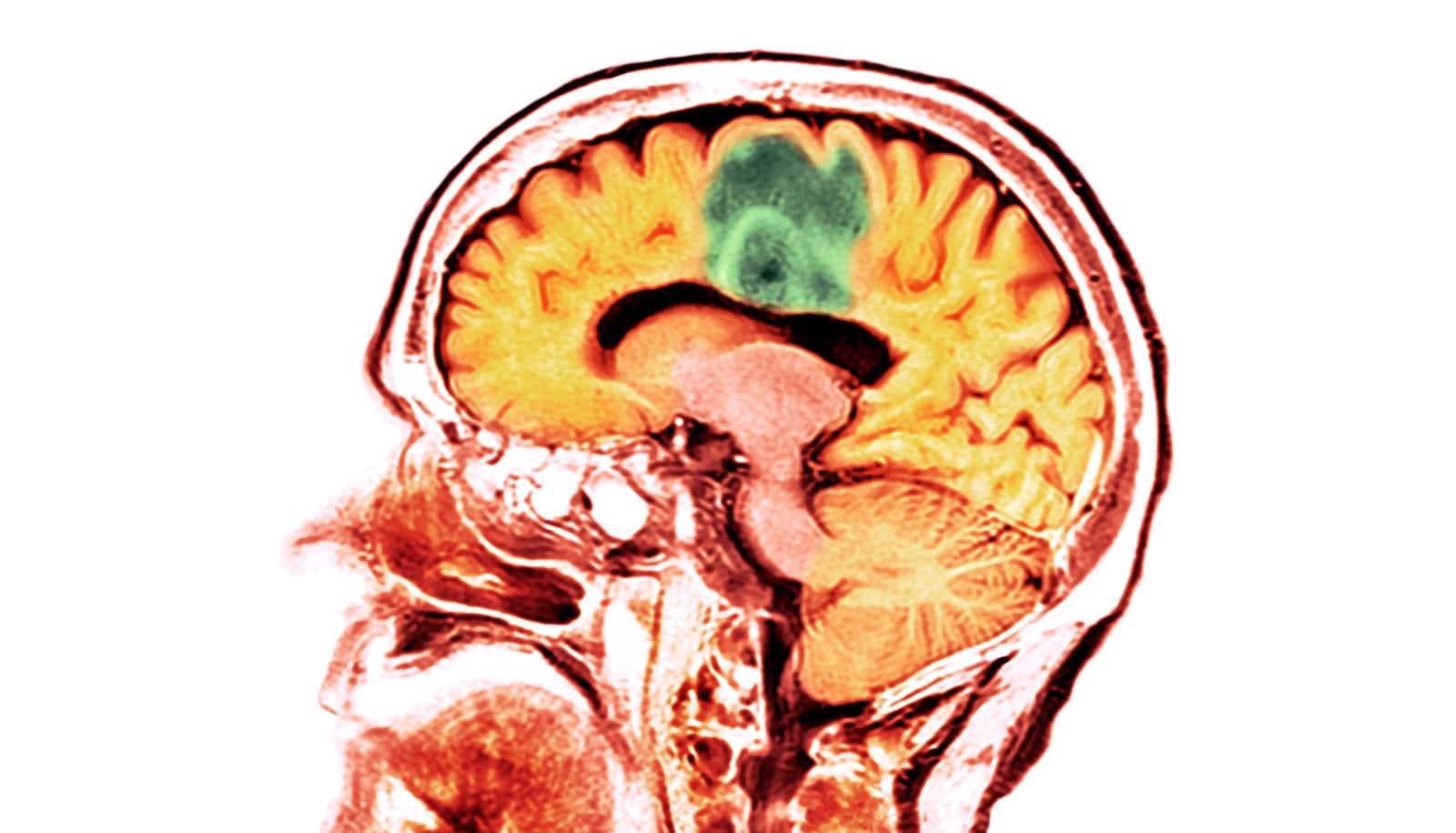
Meningiomas are tumors that arise from the membranes surrounding the brain and spinal cord. They are the most common primary central nervous system tumor, with an incidence of 8.14 per 100,000 population.
While they generally have better outcomes than other brain tumors, there is a great deal of variability in aggressiveness. Being able to predict malignancy and accurately estimate survival is therefore incredibly important in deciding whether surgery is the best option for the patient.
In this study, researchers trained machine learning algorithms on data from more than 62,000 patients with a meningioma. They used patient data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results Database. Their goal was to find statistical associations between malignancy, survival, and a series of basic clinical variables including tumor size, tumor location, and surgical procedure.
While the study demonstrates that the models could effectively predict outcomes in individual patients, the researchers emphasize the need for further refinements using larger sets that include brain imaging and molecular data.
They also developed an open-source smartphone app to allow clinicians and other researchers to interactively explore the predictive algorithms described in the paper. They hope that making the app entirely free and open source could help future projects translate newly developed machine learning algorithms to real-world clinical practice.
First author Jeremy Moreau, a PhD candidate at the Montreal Neurological Institute at McGill University, says the idea of the app was to make the predictive models accessible for the average clinician. While more work is necessary before it can be used in clinic, Moreau says putting it in the hands of doctors allows them to give suggestions that will be needed for further development.
“We have gotten great feedback on how the app can be used to explore how different clinical factors might influence malignancy and survival,” says Moreau.
“We believe it provides a unique entry-point for furthering the translatability and transparency of machine learning models, which too often remain impossible for the average clinician to evaluate because of the time and programming knowledge this would require.”
The study appears in the journal npj Digital Medicine.
Funding for the study came from the Foundation of the Department of Neurosurgery and the Canada First Research Excellence Fund. Moreau also received training awards from the Fonds de recherche du Québec—Santé (FRQS) and the Foundation of Stars.
Source: McGill University