A small, portable breath monitor can quickly and accurately detect acute respiratory distress syndrome, researchers report.
Acute respiratory distress syndrome (ARDS) is an often deadly disease that causes fluid to leak into the lungs and demands early diagnosis.
To detect the condition today, doctors rely heavily on their own judgment and time-consuming tests. The researchers say their new technology could improve survival rates and lower the cost of care.
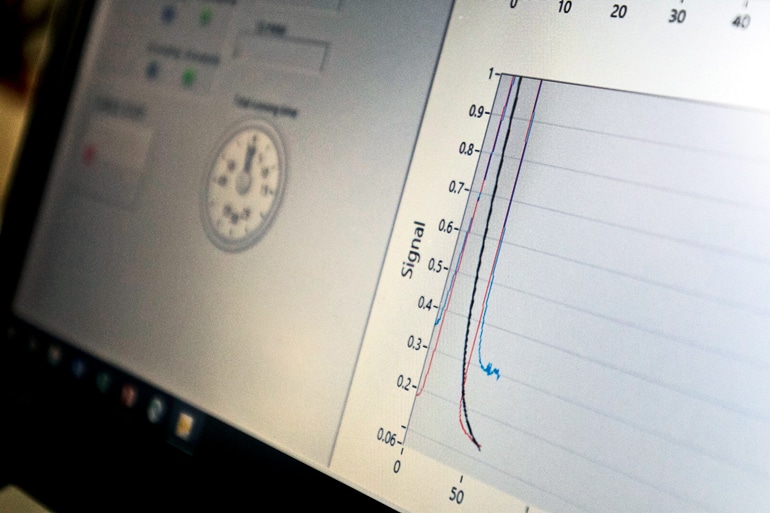
The device—a gas chromatography system—can diagnose ARDS with nearly 90% accuracy in as little as 30 minutes. In addition, its speed and cost-effectiveness allow it to essentially serve as a real-time monitor for patients, helping to focus and adjust treatments in progress. Forty-eight patient volunteers at the University of Michigan hospital, 21 with ARDS, participated in testing the device.
Better acute respiratory distress syndrome detection
“The most commonly used ARDS prediction tools are only correct about 18% of the time,” says Xudong (Sherman) Fan, a professor of biomedical engineering. “We’ve found that if our device tells us the patient is positive for ARDS, it’s highly likely that they’re positive.
“We are able to detect the onset and improvement of the condition before traditional changes in X-rays and blood testing would occur.”
ARDS is a severe state of lung inflammation that can be caused by pneumonia, sepsis, trauma, aspiration or a combination of these. It carries a high mortality rate. In the US each year, 200,000 cases are diagnosed with ARDS, resulting in 74,000 deaths.
Many that survive are left with poor lung function and have great difficulty returning to routine daily activities. There is no cure for ARDS, and mechanical ventilation in an intensive care unit is usually required to support the patient until the lung heals. Detecting it early improves patients’ outcomes.
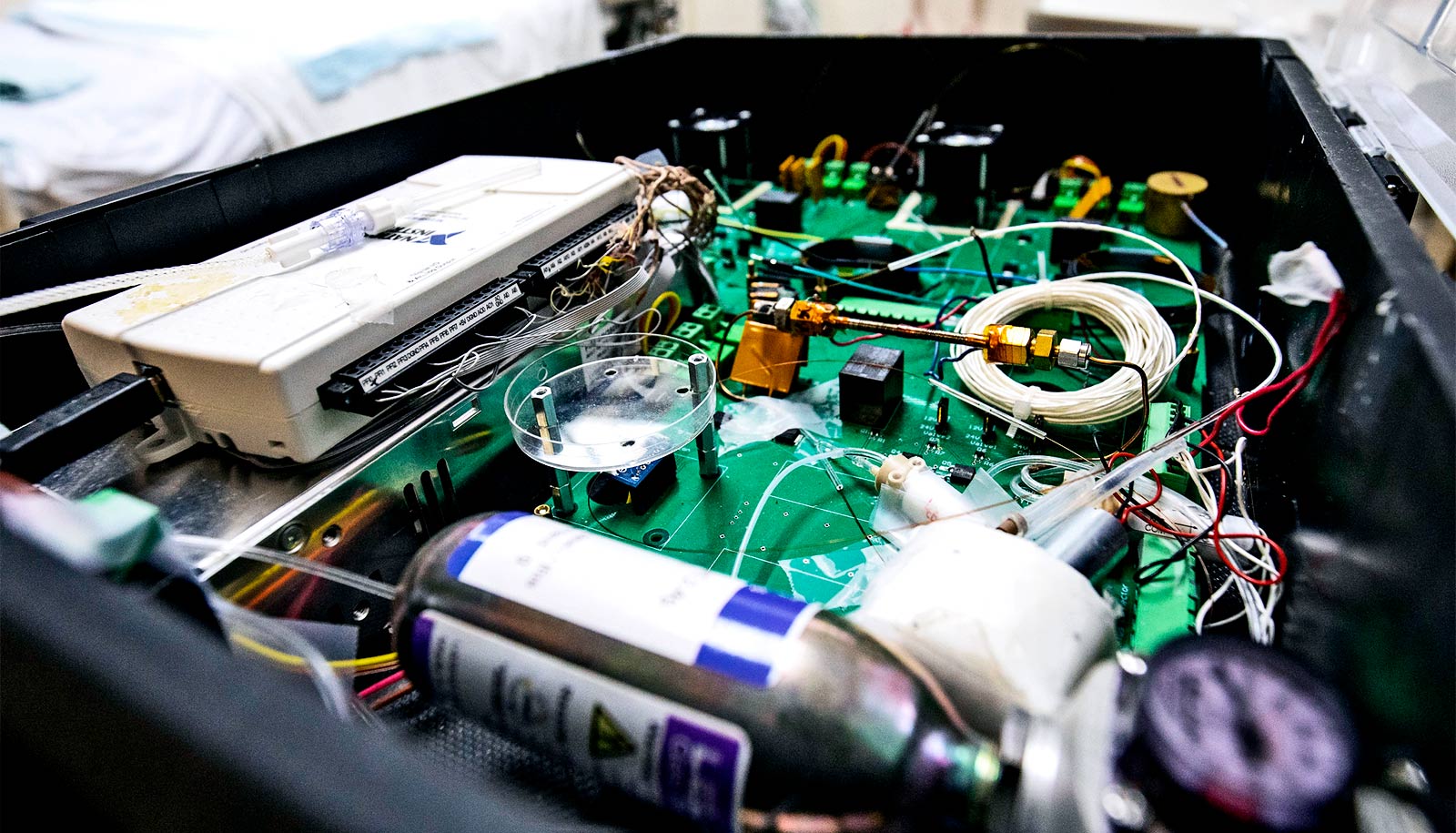
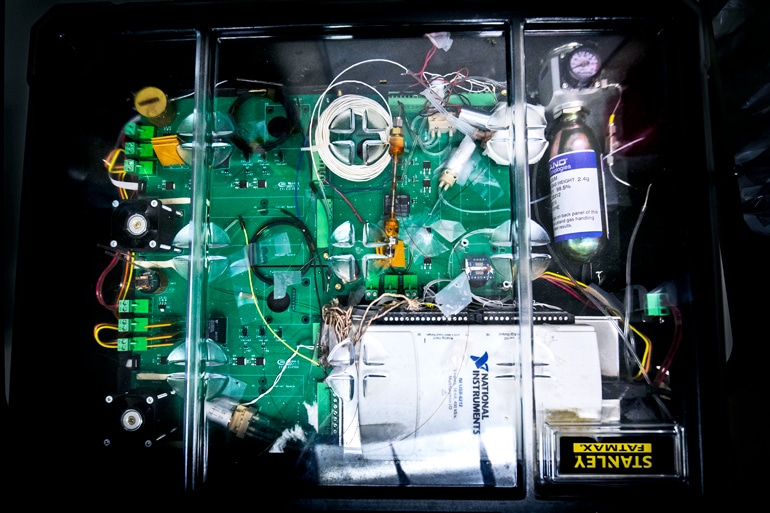
Biomarker box
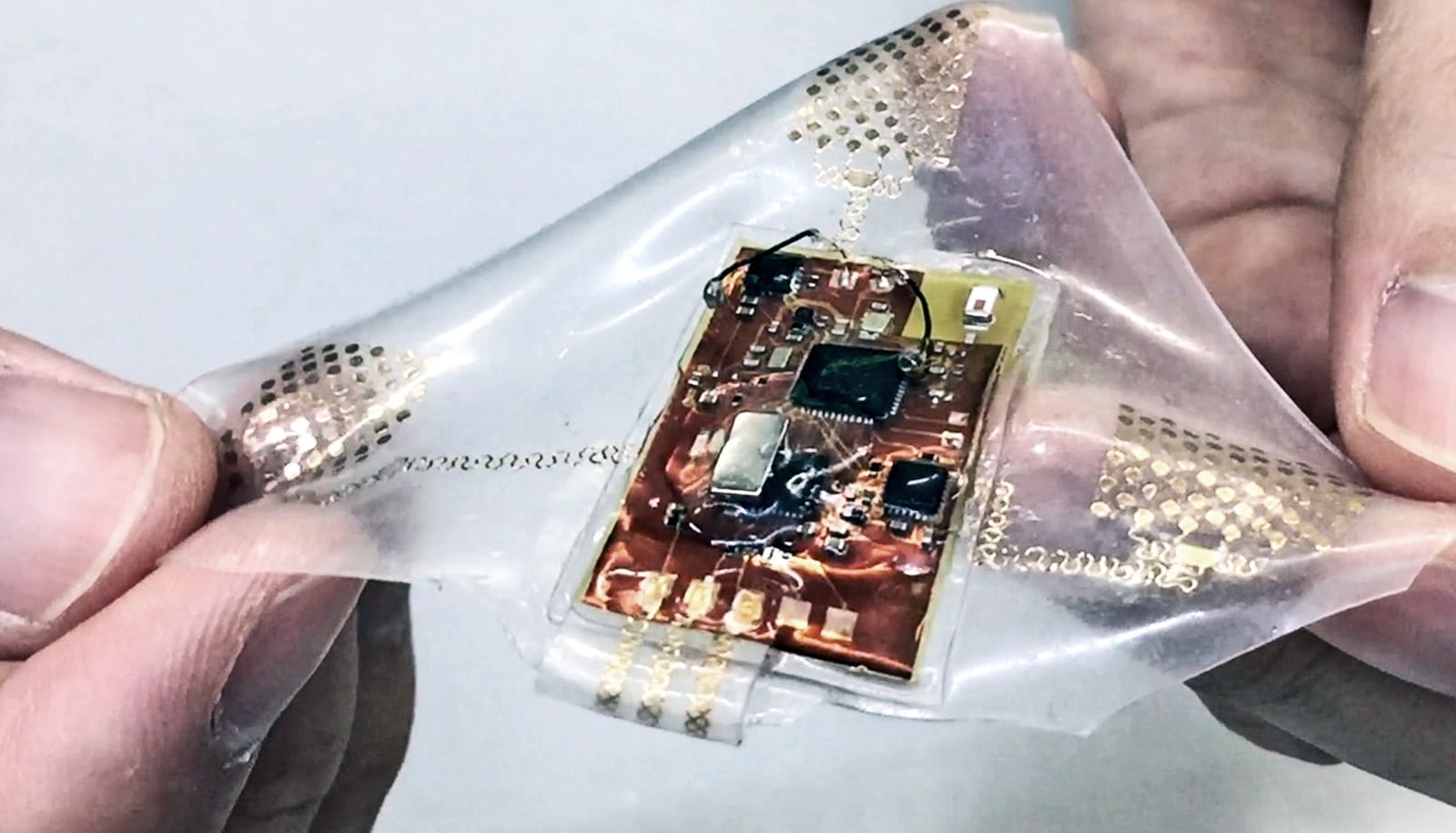
The first-of-its-kind device samples a patient’s breath through tubing connected to the exhalation port of a mechanical ventilator. It analyzes nearly 100 volatile organic compounds—biomarkers that can not only detect ARDS, but also determine how far along the disease is. As treatment begins, the device can monitor its effectiveness.
Currently, a doctor who suspects ARDS will order a chest X-ray and blood tests. The first is expensive and exposes the patient to radiation, and the second is invasive. The combination can take hours to completely analyze, and those results represent one snapshot in time. To know if the condition is improving or worsening, doctors need to repeat the tests.
“Our ability to improve outcomes with ARDS has been basically halted by the lack of technologies that can rapidly and accurately diagnose the disease early as well as track its progress,” says Kevin Ward, professor of emergency medicine and biomedical engineering. “All our current methods result in us treating the disease too late or not having information that tells us if our therapies are making a difference soon enough.
“By utilizing exhaled breath, the technology we have developed solves both problems and opens up significant opportunities to allow us to treat earlier and to develop a host of precision medicine therapies for ARDS.”
Fan and Ward see ARDS as the first of many conditions that this new technology could better identify and track.
“The technology should also be extremely useful in detecting and following the course of many other diseases such as pneumonia, sepsis, asthma, and others associated with either lung or systemic blood inflammation,” Ward says.
The research appears in the journal Analytical and Bioanalytical Chemistry.
The gas chromatography system is the result of a research and development partnership with the Michigan Center for Integrative Research in Critical Care. The University of Michigan’s FFMI MTRAC program and the National Institutes of Health supported the research. The university is pursuing patent protection for the intellectual property and is seeking commercialization partners to help bring the technology to market.
Source: University of Michigan