Compared to standard dressings, high-tech negative pressure wound therapy devices don’t improve patient recovery from open leg fractures, new research shows.
This study involved people with an “open” fracture of the leg, where the bone has broken through the skin. The broken bone is exposed to contamination and there is a higher risk of healing-related complications. In severe open leg fractures, infection rates can be as high as 27 percent. As well as affecting the recovery of the patient, infections can also increase healthcare costs due to longer hospital stays or extra treatments.
“Our study did not find any benefit of using negative pressure devices in the treatment of these very serious injuries,” says lead author Matt Costa, professor of orthopedic trauma surgery in the Nuffield department of orthopedics, rheumatology, and musculoskeletal sciences at the University of Oxford. “Our research has implications for both patients and healthcare systems with regard to the management of severe open fractures.”
The randomized clinical trial took place at the University of Warwick Clinical Trials Unit and the University of Oxford across 24 hospitals representing the UK Major Trauma Network. The results appear in the Journal of the American Medical Association.
Negative-pressure wound therapy (NPWT) is a new type of dressing used after surgery. The device creates a vacuum using a suction pump that removes blood and fluid that may collect in a wound. The vacuum may also encourage the formation of granulation (healing) tissue. However, NPWT dressings and the vacuum machines are considerably more expensive than traditional wound dressings.
The researchers compared the level of disability, rate of infection, and quality of life in 460 patients (the mean age was 45.3 years and 73 percent were men) with severe open fractures of the lower leg. It was not possible to do a “blind” study of the participants and surgeons because the type of dressing was clearly visible. However the surgical and healthcare team was not involved in any outcome assessments. The primary method of measurement was a questionnaire that the patients used to rate their level of disability one year after they sustained their injury.
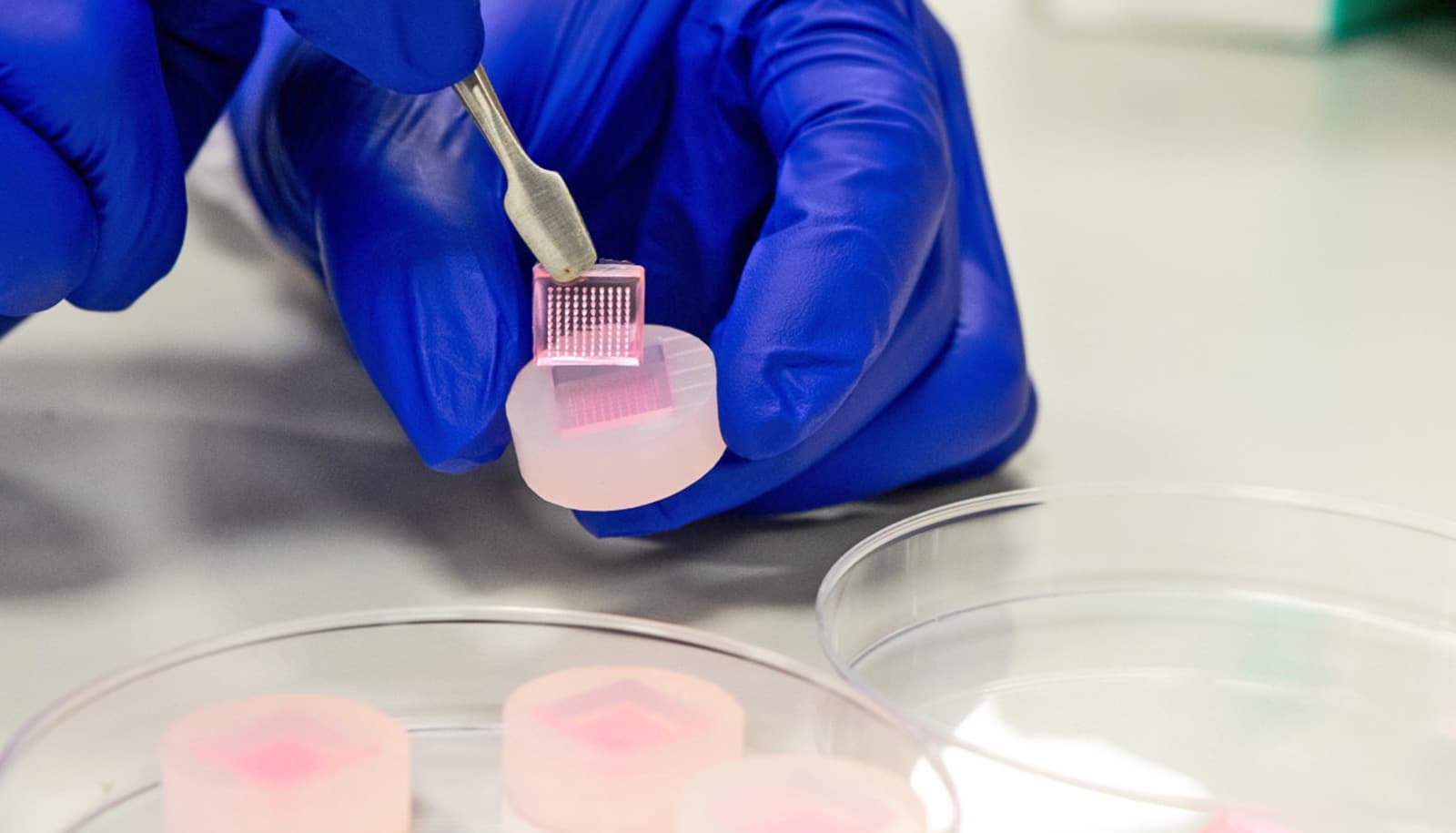
Injectable bandage could save lives on the battlefield
The research team found no evidence that the negative pressure wound devices reduced the patients’ disability at 12 months. The questionnaire results were 45.5 (negative pressure) vs. 42.4 (standard dressings) points out a possible 100 where zero represents normal function and 100 complete disability. Independent clinicians, who were not told which dressing was used, reviewed photos taken of the wounds at six weeks. The research team found there was no evidence of a difference in the rate of deep infections, wound healing, or patient quality of life.
“Before this study there was only one small randomized clinical trial comparing standard wound dressings with the devices which suggested negative-pressure wound therapy improved patient outcomes. However it was conducted at one trauma centre and only included 59 patients,” says coauthor Julie Bruce, professorial fellow at Warwick Medical School. “Despite the lack of strong evidence, clinical guidelines around the world recommended the use of these devices for open fracture wounds. These guidelines will need updating.”
Source: University of Warwick