Mice are more susceptible to severe West Nile disease if they’ve recently taken antibiotics that change the makeup of their gut bacterial community, new research indicates.
Doctors recommend against taking antibiotics for viral infections because antibiotics don’t kill viruses, but do promote antibiotic resistance. The findings suggest another reason not to take antibiotics: taking antibiotics for viral infections may increase susceptibility to later infection.
People infected with West Nile virus can show a wide range of disease. Some develop life-threatening brain infections. Others show no signs of infection at all. One reason for the different outcomes may lie in the community of microbes that populate their intestinal tracts.
“The immune system is activated differently if the gut does not have a healthy microbiome,” says senior author Michael S. Diamond, professor of medicine at Washington University in St. Louis.
“If someone is sick with a bacterial infection, they absolutely should take antibiotics. But it is important to remember that there may be collateral effects. You might be affecting your immune response to certain viral infections.”
Different responses
West Nile virus is not unusual in its ability to cause disease ranging from mild to severe. Many viral infections cause no symptoms in the majority of people, mild to moderate disease in some, and severe disease in an unlucky few.
But why people respond so differently to the same organism has never been entirely clear. Human genetics doesn’t explain everything, and neither does the genetic makeup of the microbe itself, although both play a role.
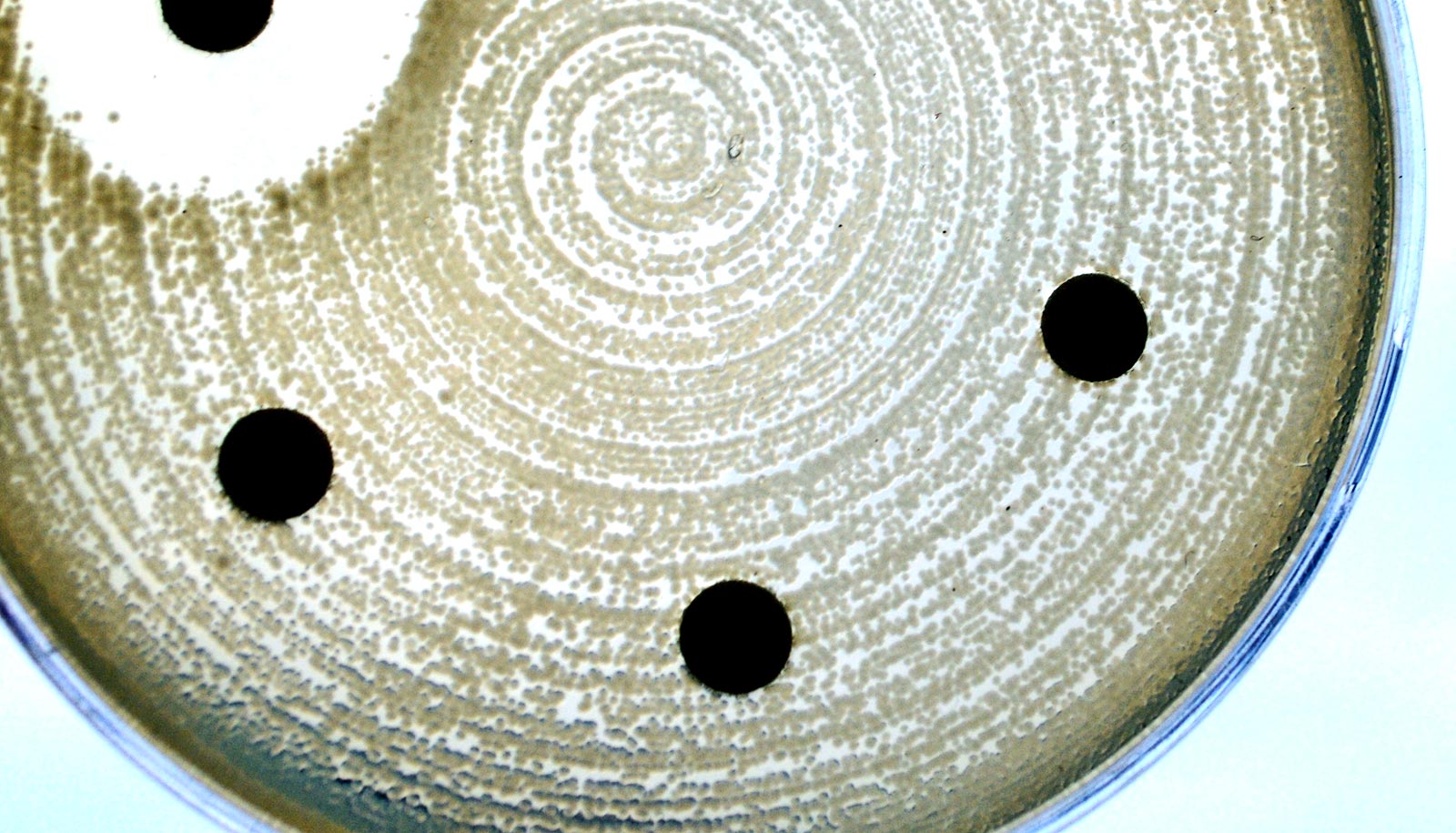
As reported in Cell Reports, researchers set out to determine whether antibiotic use could help explain why some people get very sick and others don’t. Antibiotics kill off members of the normal bacterial community and allow some potentially harmful ones to overgrow.
Since a healthy immune system depends on a healthy gut microbiome, antibiotics may be hobbling the immune system, leaving the body unprepared to fight off a subsequent viral infection.
Researchers gave mice a placebo or a cocktail of four antibiotics—vancomycin, neomycin, ampicillin, and metronidazole—for two weeks before infecting the mice with West Nile virus. About 80 percent of the mice that received no antibiotics survived the infection, while only 20 percent of the antibiotic-treated mice did.
Subsequent experiments showed that the mice stayed at high risk for more than a week after the antibiotic treatment ended, and just three days of antibiotic treatment was enough to raise the mice’s risk of dying from West Nile infection.
To find out whether increased susceptibility to viral infection was linked to changes in gut bacteria, the researchers tested the four antibiotics separately and in combination. Treatment with ampicillin or vancomycin alone made the mice more likely to die of West Nile, while neomycin did not. Metronidazole had no effect alone, but it amplified the effect of ampicillin or vancomycin.
Further, different antibiotic treatments led to changes to the bacterial community in the gut that correlated with vulnerability to viral infection.
“Once you put a dent in a microbial community, unexpected things happen,” says first author Larissa Thackray, assistant professor of medicine. “Some groups of bacteria are depleted and different species grow out. So increased susceptibility may be due to both the loss of a normal signal that promotes good immunity and the gain of an inhibitory signal.”
Weak T cell response
The researchers tested immune cells from mice they treated with antibiotics and found that they had low numbers of an important immune cell known as killer T cells. Normally, during an infection T cells that recognize the invading virus multiply to high numbers and play a critical role in controlling the infection. Mice researchers treated with antibiotics generated fewer such T cells.
Lay off the antibiotics for these small infections?
“It’s likely that antibiotic use could increase susceptibility to any virus that is controlled by T cell immunity, and that’s many of them,” Thackray says.
The weak T cell response is likely a byproduct of the changes to the bacterial populations the antibiotics caused, not a direct effect of the drugs on the immune cells. For one thing, the mice still had trouble fending off viral infection a week or more after they stopped receiving antibiotics. For another, transferring gut bacteria from mice given antibiotics to other antibiotic-treated mice made the recipients even more vulnerable to viral infection, suggesting that something in the bacteria was undermining the mice’s immune response.
Antibiotics can goad ‘superbugs’ into ganging up on us
Researchers need to confirm the study in people, whose microbiota normally contains a different collection of bacteria than mice’s. Still, the findings suggest that taking antibiotics unnecessarily may be unwise.
“There’s a number of people who get sick, some more than others, for reasons we don’t understand,” says Diamond, who is also a professor of molecular microbiology, and of pathology and immunology.
“If your immune system doesn’t get activated because your microbiome is perturbed by antibiotics or anything else—diet, other infections, underlying medical conditions—you may be at higher risk of severe viral disease.”
The National Institutes of Health and the Center for Women’s Infectious Disease Research funded the work.