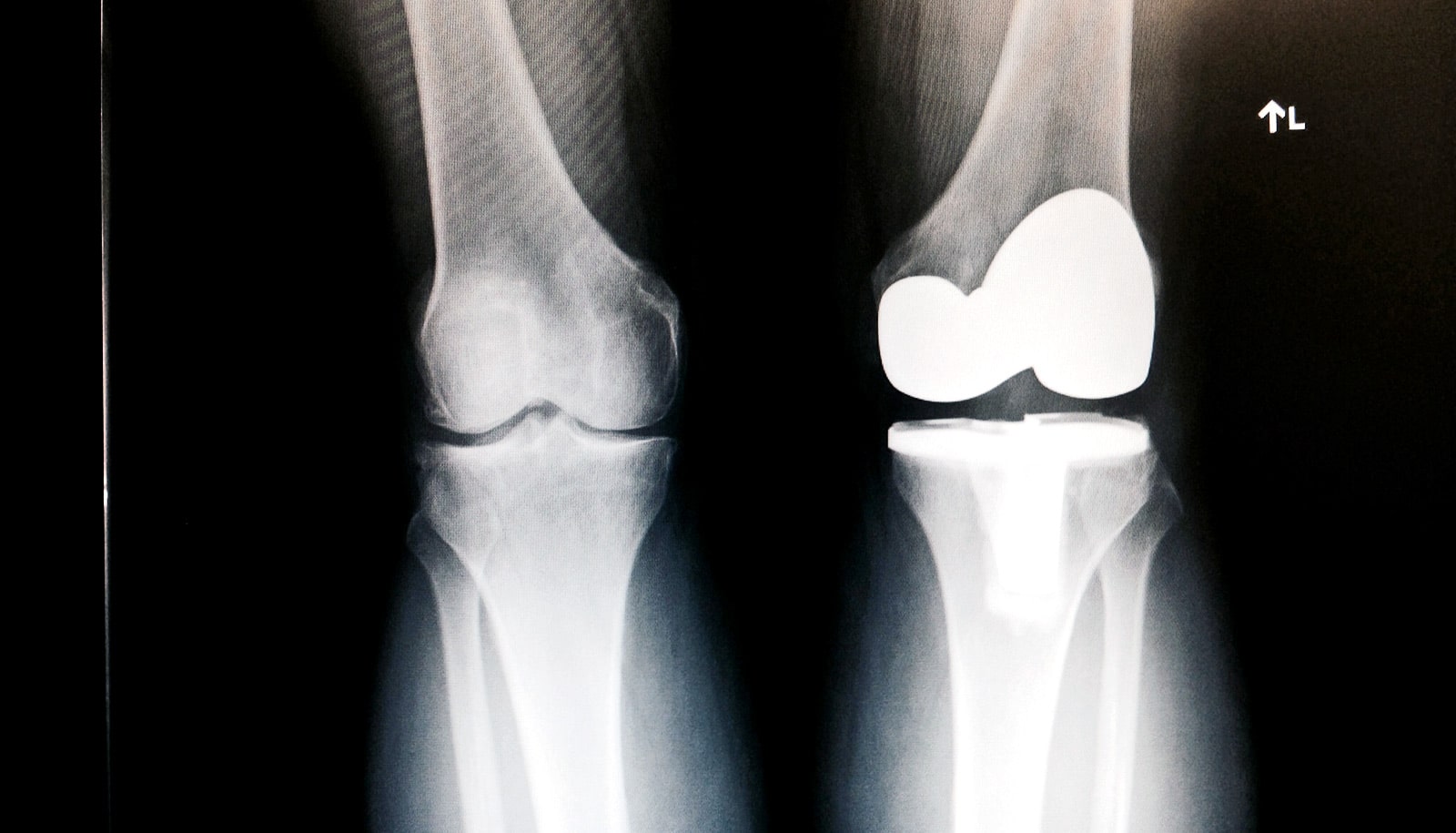
A new study recommends an alternative method of pain relief for patients undergoing knee replacement surgery.
Over 250 patients having knee replacements at University Hospitals Coventry and Warwickshire (UHCW) took part in the study, which appears in the Bone and Joint Journal.
“This is to be welcomed as the potential risks of morphine-type pain relief are well known…”
A traditional option for pain relief during knee replacement surgery is a ‘femoral nerve block’; a single dose of local anesthetic injected around the femoral nerve in the groin, which is typically administered by an anesthetist.
A newer alternative approach, however, uses an injection of anesthetic agents around the knee joint and is administered by the surgeon without the need for specialist equipment.
The study found that patients who had the knee injections required lower doses of powerful painkillers such as morphine after surgery. Morphine can cause serious and troublesome side effects in postoperative patients and is best avoided if possible.
Clipping cartilage after knee surgery doesn’t help
Also, unlike a femoral nerve block, there is no need for specialist equipment like ultrasound. This is therefore likely to save surgeons and anesthetists valuable time and resources and improve patient care.
“Our study has demonstrated the advantages of injections of anesthetic agents around the knee during knee replacement surgery over other methods,” says Peter Wall, lead author of the report and a clinical lecturer at UHCW NHS Trust and the University of Warwick.
“These injections are now shown to be safe and effective. They also involve fewer resources and reduce the need for powerful painkillers such as morphine,” he says.
“This is to be welcomed as the potential risks of morphine-type pain relief are well known and should be avoided where possible. We hope that these study findings, if put into practice, will benefit patients around the world.”
Gold gives titanium knees extra strength
The National Institute for Health Research (NIHR) Research for Patient Benefit (RfPB) Programme funded the study.
Source: University of Warwick