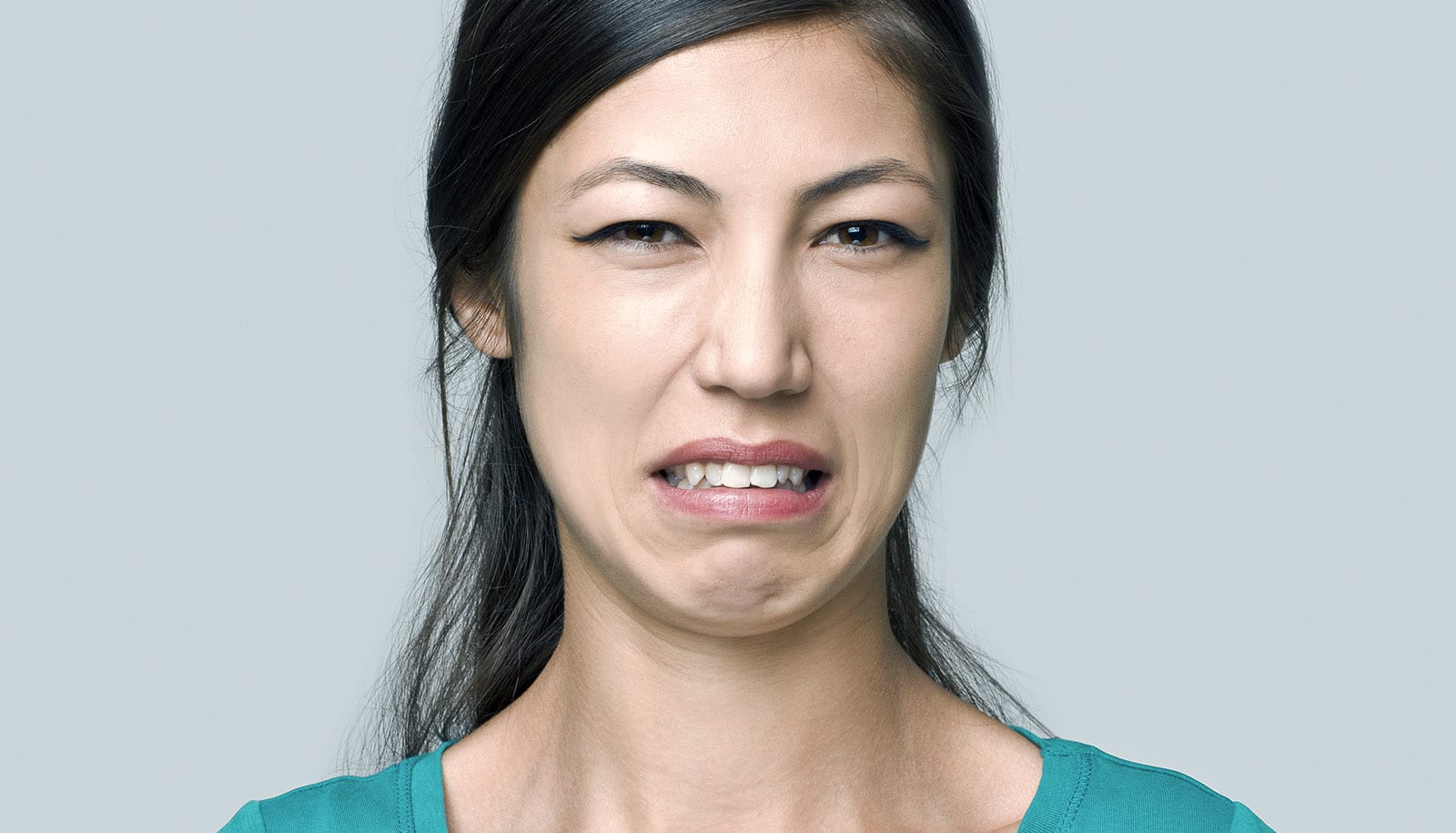
Tiny droplets of saliva can carry bacteria from the mouth to the lungs, a new study shows. That means bacteria are able to avoid the epiglottis, the movable tissue barrier that keeps most saliva from getting into the lower respiratory tract.
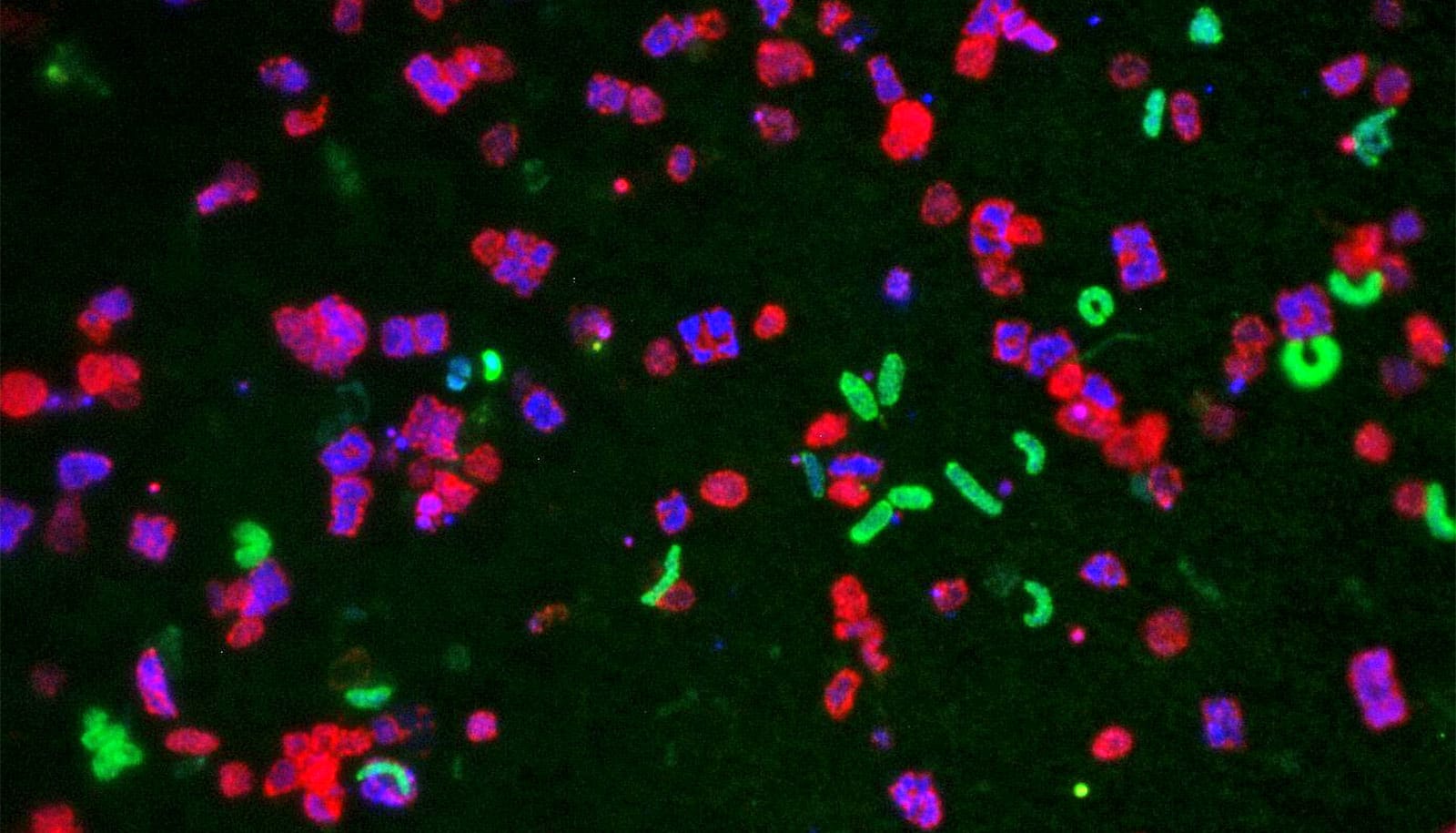
By studying the DNA of these bacteria in the lungs of healthy volunteers, researchers confirmed that the population of microbes in the lungs closely resembles the population found in the mouth. And by studying the microbes’ distribution within the airways, the researchers could determine their most likely entry route.
They found that many of the immigrant microbes make their home near the main carina, the spot at the end of the trachea where the airway branches off to the left and right lungs. This spot in the lungs is a “landing pad” where aspirated saliva—because of gravity and our upright posture—is likely to collide with the airway. But some bacteria manage to make it all the way to the deepest reaches of the pulmonary system and reside in the tiny air sacs called alveoli.
Wherever the bacteria land, they join a community made up mostly of other recent immigrants. Few microbes are thought to be long-term residents of healthy lungs. Unlike the gut, healthy lungs are an inhospitable environment for bacteria, with little nutrition and constant surveillance by the immune system.
“This is the most comprehensive topographic survey of the healthy lung microbiome to date. It adds to the evidence that healthy lungs are like an island whose population is determined by the balance of immigration and elimination of species: who moves in and who moves out,” says Robert P. Dickson, assistant professor of internal medicine at the University of Michigan. “The microbiome of the lung plays by a different ecologic rulebook than the gut microbiome, and this study helps clarify what those rules are.”
Bacteria in your mouth may trigger arthritis
Inspired by classic models of ecology, researchers propose an “adapted island model” of the lung microbiome, in which the competing pressures of microbial immigration and elimination determine the lung’s ecosystem.
The new paper, published in the journal mBio, doesn’t just describe the lung microbiome ecosystem; it also shows that scientists who want to study it in the future can feel confident using the standard techniques doctors already use to look for lung disease.
Researchers conducted the study with eight healthy volunteers who underwent bronchoscopy at VA Ann Arbor Healthcare System.
’30 times the size of the skin’
The team obtained the lung bacteria using two techniques to sample nine separate sites in the lungs of each volunteer. One technique, called protected specimen brushing, used a special catheter that keeps bacteria from the mouth and throat from contaminating the samples taken in the airways.
Suspicion of such contamination has kept some researchers from fully accepting the results of previous lung microbiome research. So to test for this contamination, the researchers took one sample on a brush held in the middle of the airway and the rest using brushes that they gently touched to the airway wall.
The researchers got other samples through bronchoalveolar lavage, in which they squirt a small amount of fluid into the deepest part of the lung and suction it back into the bronchoscope, bringing microbes along with it. They then analyzed the bacterial DNA found in all these samples.
“We found no evidence of upper respiratory tract bacteria in these contamination control specimens,” says Dickson. “This reassured us that the rest of our samples truly reflected lung bacteria and not just contamination from the procedure” brought in by the bronchoscope as it passed through the throat.
Can anesthesia protect lungs from the flu?
Taken together, the results suggest bronchoscope-based techniques can be used to study the lung microbiome—in sickness and in health.
“The lungs are our largest interface with the outside environment, with 70 square meters of surface area,” says Dickson. “That’s 30 times the size of the skin and twice the size of the gastrointestinal tract. And this study confirms that they’re under constant bombardment by diverse communities of bacteria.”
The researchers emphasize that these volunteers were healthy and had no symptoms that suggested pneumonia or other respiratory disease. “These volunteers were as healthy as you or me,” Dickson says. “We are probably all aspirating small amounts of bacteria constantly, and so long as our immune system is intact, they rarely make us sick.”
Microaspiration in healthy people has been observed for nearly a century in studies using medical imaging techniques. “We’ve known about the existence of microaspiration for decades,” says Dickson. “But this is the first time we’ve been able to find its ecologic fingerprint.”
Next steps in the research will include what happens in people who have problems with the elimination part of this equation.
‘Diseased lungs are more like a tropical island’
Inability to cough irritants out of the lung, or to carry them out through the sweeping action of hairlike cilia on lung cell surfaces, could lead to more microbes staying longer in the lungs than normal. And that could lead to a higher risk of lung infection.
Such research could lead to better understanding of the lung microbiome’s importance in conditions such as chronic obstructive pulmonary disease, cystic fibrosis, and the types of lung failure seen in intensive care units.
“If healthy lungs are like Antarctica—where conditions aren’t good for reproduction— then diseased lungs are more like a tropical island, where lower rates of elimination and altered environmental conditions permit the persistence and reproduction of certain bacteria,” he says.
How spit protects us from poison in coffee
Dickson also thinks it would be interesting to study how the lung microbiome changes when a person has a viral infection that causes the upper respiratory tract to produce more nasal secretions. “I certainly look at my kids with their constantly runny noses and wonder if their lung microbiome looks more ‘nasal’ than ‘oral.'”
And as researchers begin to uncover the impact of common medications such as antibiotics and proton pump inhibitors on the microbiome in the digestive system, he notes that it’s not unreasonable to think that these drugs also affect the lung microbiome. He and colleagues have already found evidence that the lungs are filled with gut microbes in critically ill patients.
The research was sponsored by the National Institutes of Health and the Department of Veterans Affairs, as well as the Michigan Institute for Clinical & Health Research, the U-M Medical School’s Host Microbiome Initiative, and the Michigan Center for Integrative Research in Critical Care.
Source: University of Michigan