3D cultures of neural cells that model basic properties of the brain produce networks of capillaries, research shows.
The networks of capillaries within the little balls of nervous system cells could enable new kinds of large-scale lab investigations into diseases, such as stroke or concussion, where the interaction between the brain and its circulatory system is paramount, says Diane Hoffman-Kim, senior author of the study in the Journal of Neuroscience Methods.
More fundamentally, vasculature makes mini-brains more realistic.
“This is exciting because real brains have vasculature,” says Hoffman-Kim, an associate professor of medical science and of engineering at Brown University. “We rely on it. For our neurons to do their thing, they have to be close to some blood vessels. If we are going to study lab models of the brain, we would love for them to have vasculature, too.”
Because scientists can make them by the hundreds, mini-brains hold promise not only for advancing medical and scientific research, but also for doing so with less need for animal models. Hoffman-Kim’s lab first described its mini-brain method in 2015. While the engineered tissues appeared relatively simple compared to some others, they were also relatively easy and inexpensive to make.
‘Tangles of spaghetti’
But what had remained unnoticed at the time, even by the inventors, was that the little 8,000-cell spheres cultured from mouse cells were capable of growing an elementary circulatory system.
Only as members of the lab including lead author and Brown Graduate School alumna Molly Boutin continued to work with and study the mini-brains did they discover that after about day three of culture, about two-thirds of the mini-brains had grown networks of non-neural tissue. Closer inspection revealed that these tangles of spaghetti were self-assembled (i.e. they just grew) tubes made of the cells and proteins found in blood vessels.
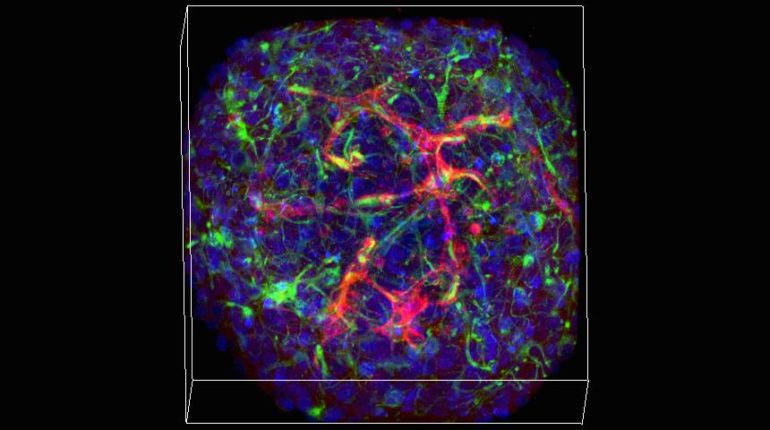
The new study features a wide variety of imaging experiments in which staining and fluorescence techniques reveal those different cell types and proteins within the mini-brain spheres. The study also documents their integration with the neural tissues. Cross-sections under a transmission electron microscope, meanwhile, show that the capillaries are indeed hollow tubes that could transport blood.
Capillaries scramble to feed oxygen to the brain
Of course, there is no blood in a tiny mini-brain, Hoffman-Kim says. They exist in an agarose wellplate, not in a living animal. But she’s currently working with a colleague at Brown to design a way to connect the mini-brains with a microfluidic apparatus that could produce an external source of circulation through a mini-brain.
The capillary networks are not as dense as they would be in a real brain, she acknowledges. The study also shows that they don’t last longer than about a week or two.
Mini-brain experiments
Aware of both their constraints and their potential, Hoffman-Kim’s lab has already started experiments to take advantage of the presence of vasculature. Study second author Liana Kramer, a Brown senior, has begun looking at what happens to the vasculature and neural cells when mini-brains are deprived of oxygen or glucose. Later that same test bed could be used to examine the difference that different drugs or other treatments make.
Could 3D printing keep lab-grown organs alive?
Vasculature is particularly important not only because it delivers oxygen, glucose, and medicine to brain cells, but also because research shows that in strokes, Alzheimer’s disease, and brain injury, the brain sometimes attempts to redesign its vasculature to compensate for what’s happening to it. The mini-brains could allow researchers to observe such responses amid different lab-created conditions and treatments, Hoffman-Kim says.
“We can study a range of injury conditions, several drugs that are being tested and several conditions—such as stroke and diabetes—together,” she says.
Funding from the National Science Foundation, NIH, Brown University, Brown alumni Donna McGraw Weiss and Jason Weiss, and the Association of Migraine Disorders supported the research.
Source: Brown University



