A new 3D printing method can create a life-size human hand in 19 minutes—instead of six hours using conventional 3D printing.
It’s a step toward creating 3D printed human organs and tissue, researchers report.
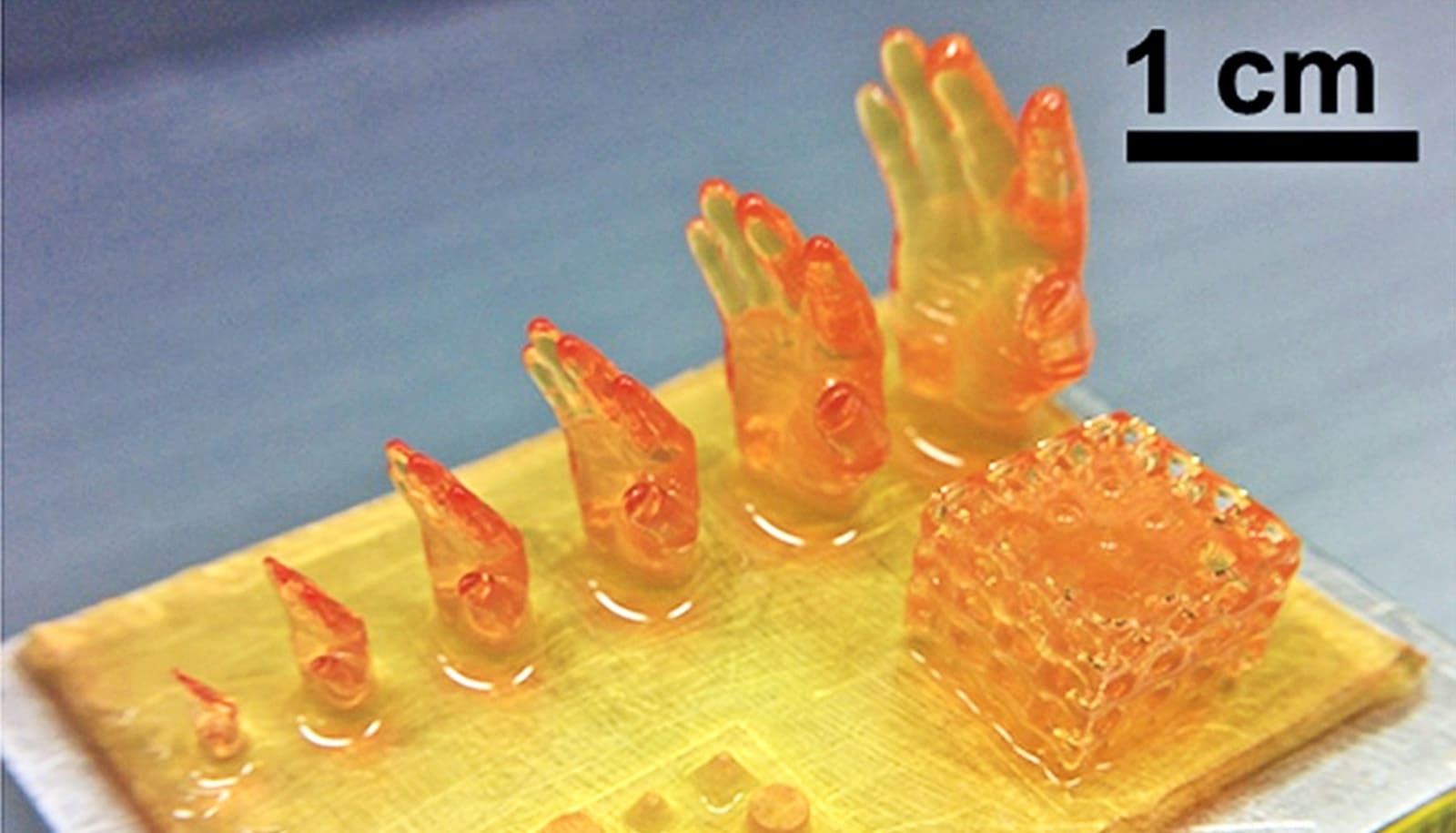
It looks like science fiction: A machine dips into a shallow vat of translucent yellow goo and pulls out what becomes a life-sized hand. But it’s real—and the biotechnology could eventually save countless lives lost due to the shortage of donor organs, researchers say.
“The technology we’ve developed is 10-50 times faster than the industry standard, and it works with large sample sizes that have been very difficult to achieve previously,” says Ruogang Zhao, associate professor of biomedical engineering at the University at Buffalo and co-lead author of a paper on the technique in Advanced Healthcare Materials.
The work centers on a 3D printing method called stereolithography and jelly-like materials known as hydrogels, used to create, among things, diapers, contact lenses, and scaffolds in tissue engineering.
The latter application is particularly useful in 3D printing, and it’s something the research team spent a major part of its effort optimizing to achieve its incredibly fast and accurate 3D printing technique.

“Our method allows for the rapid printing of centimeter-sized hydrogel models. It significantly reduces part deformation and cellular injuries caused by the prolonged exposure to the environmental stresses you commonly see in conventional 3D printing methods,” says co-lead author, Chi Zhou, associate professor of industrial and systems engineering.
Researchers say the method is particularly suitable for printing cells with embedded blood vessel networks, a nascent technology expected to be a central part of the production of 3D-printed human tissue and organs.
The researchers have filed a provisional patent of the technology, and have formed a startup company, Float3D, to commercialize the technology.
Additional coauthors are from the VA Western New York Healthcare System, Roswell Park Comprehensive Cancer Center, Syracuse University, and the University at Buffalo.
The National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health and the University at Buffalo School of Engineering and Applied Sciences and the Jacobs School of Medicine and Biomedical Sciences funded the work.
Source: University at Buffalo