Researchers have identified a new way to predict which patients who have received transcatheter aortic valve implantation may be at risk for hospital readmission for heart failure.
“Heart failure readmission is one of the most common cardiac-related readmissions within the first year after TAVR…”
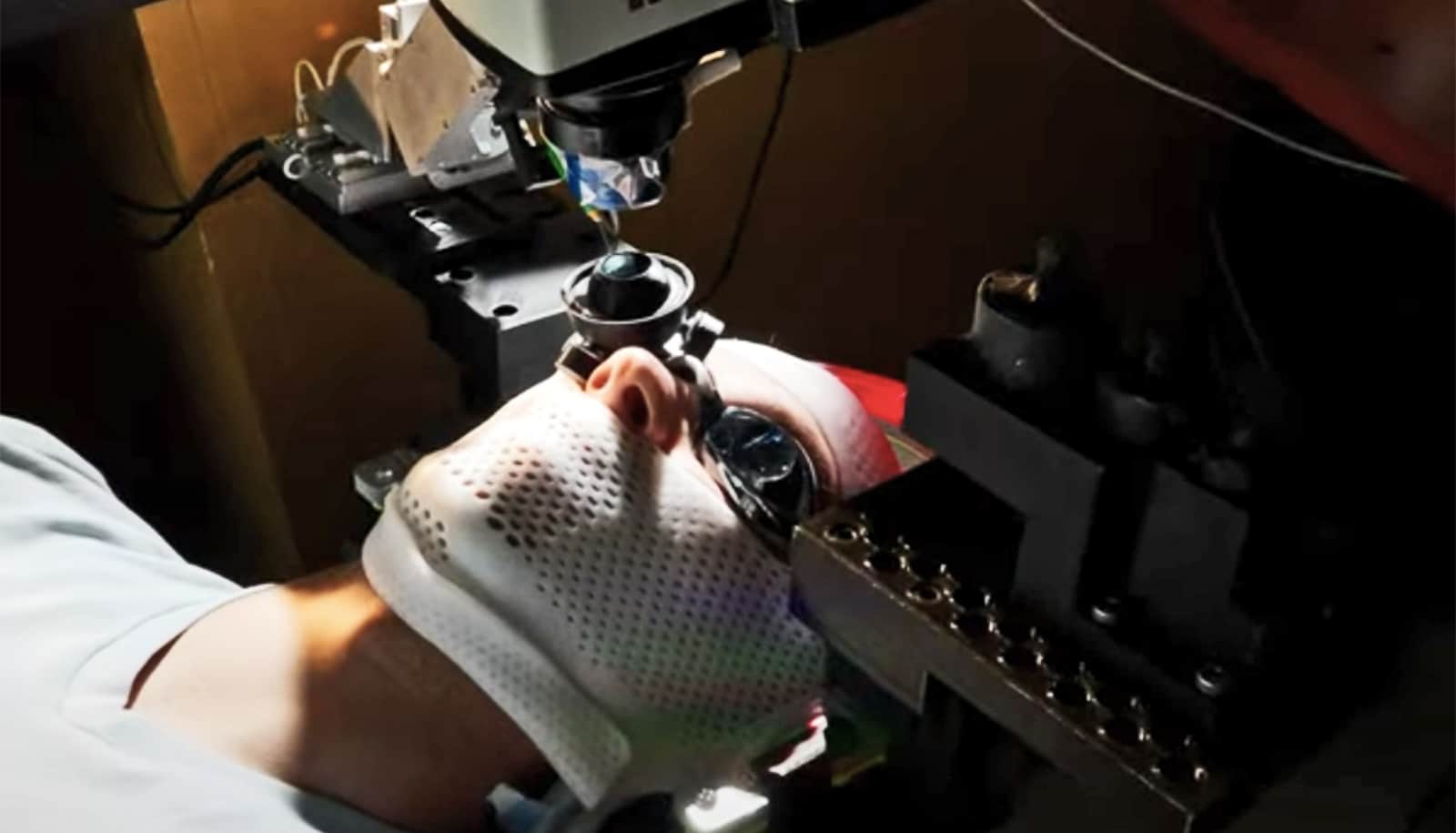
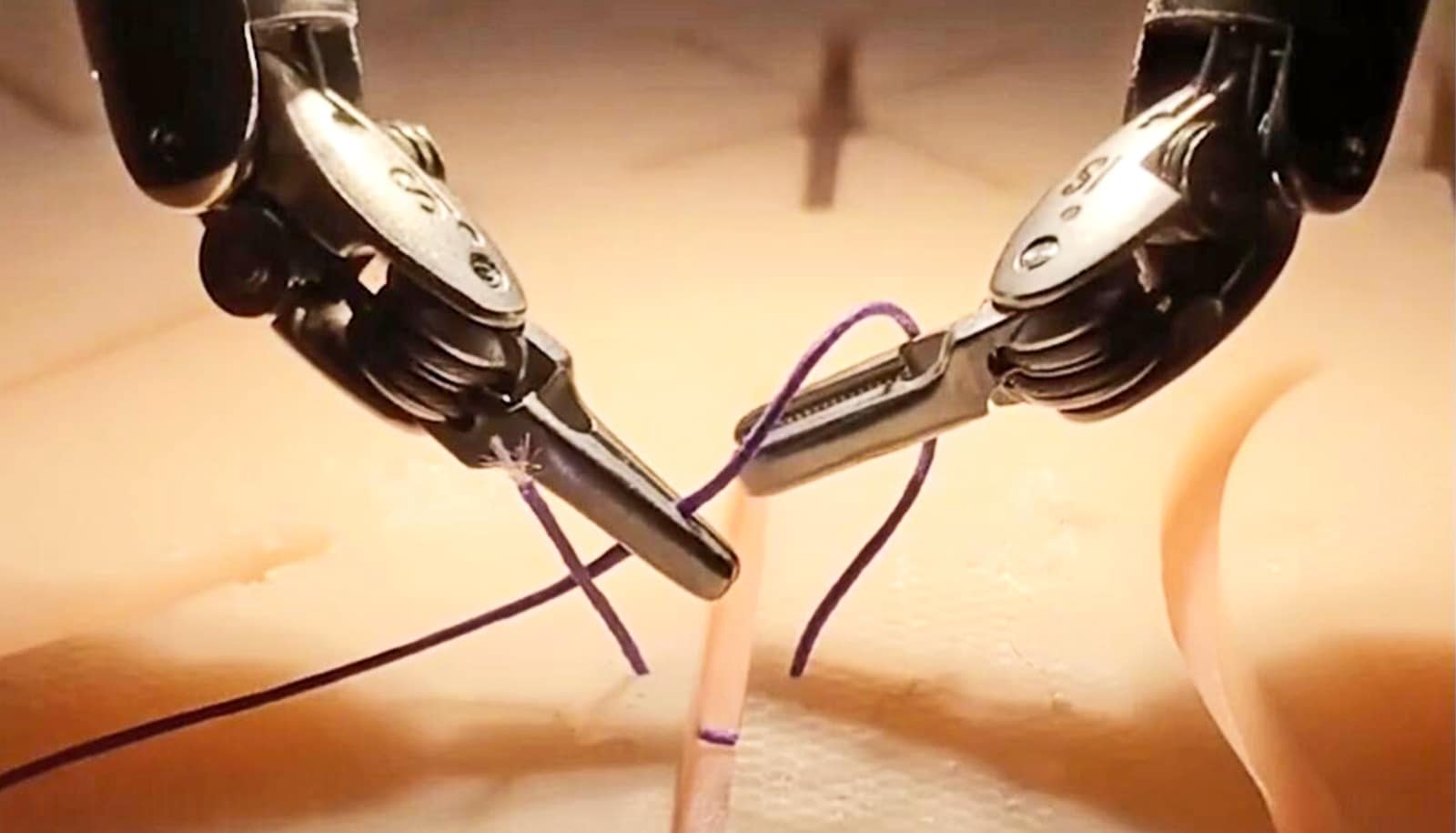
TAVR is a minimally invasive procedure reserved for patients who have been turned down for a traditional aortic valve replacement by open heart surgery due to serious medical co-morbidities.
“For many patients, TAVR is a life-saving and life-enhancing procedure and most see significant improvements in their symptoms,” says Aishwarya Bhardwaj, first author of the paper and a medical resident at the Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo.
“However, a small percentage may not benefit adequately with the procedure. Heart failure readmission is one of the most common cardiac-related readmissions within the first year after TAVR,” she explains.
The paper appears in Structural Heart: The Journal of the Heart Team.
Finding a marker
To find out what might be putting these patients at higher risk, Bhardwaj and her colleagues conducted a retrospective study on 198 patients (mean age was 82 years) who underwent TAVR from 2012-16 at the Gates Vascular Institute in Buffalo.
They focused on a measure called elevated valvuloarterial impedance, also known as Zva, which is obtained noninvasively by a cardiac ultrasound. Zva incorporates both the aortic valve stenosis and the resistance encountered by the heart due to thickening of the arteries and blood vessels for pumping blood in the body.
While Zva has been shown to have prognostic significance in TAVR patients, there was no quantifiable data as to how useful it might be in predicting heart failure, Bhardwaj explains.
“Our study was the first to evaluate the role of Zva, which can be easily obtained noninvasively for predicting heart failure readmissions,” she says. “Identifying such prognostic markers would help reduce rehospitalizations and would eventually translate into reduced health care expenditures as well.”
3D printing helps predict if new heart valves will leak
The new study found that among 41 patients who were rehospitalized after TAVR, nearly twice as many patients (34.2 percent vs. 18.1 percent) with a high Zva prior to undergoing TAVR were readmitted to the hospital after TAVR because of heart failure symptoms.
Another key finding was that patients in whom the Zva either increased or remained unchanged were three times more likely (18.2 percent vs. 6.3 percent) to die within one year of the procedure.
“For that reason, we recommend that Zva should be integrated as part of routine follow up post-TAVR,” Bhardwaj says, “and should be obtained serially during follow-up echocardiograms (ultrasounds of heart) for monitoring risk of heart failure readmissions.”
Identifying risk
Bhardwaj and her coauthors note that Zva may also have relevance to determining who should and should not undergo TAVR in the first place.
“Our findings suggest that Zva may play a key role in patients who fail to have clinical improvement post-TAVR and will most likely not benefit from the procedure,” she says, “so Zva has prognostic implications in evaluating patients who may or may not benefit with the procedure.”
The importance of such risk stratification has a significant impact, the authors says, as hospital administrations nationwide work to minimize heart failure readmissions while trying to identify patients at higher risk to utilize more resources in the outpatient setting.
This existing drug could keep heart valves bendy
“Zva can be utilized to identify patients at high risk for readmissions and accordingly, help divert resources to these patients by establishing transitional care programs and close cardiologist follow up in order to avoid readmissions in hospital,” Bhardwaj concludes. “This should translate to potential cost-savings and reduced health care expenditures.”
The researchers are now incorporating the Zva with novel indices on echocardiography on patients undergoing TAVR at the Gates Vascular Institute.
Source: University at Buffalo