A minimally invasive form of the surgery used to treat severe pancreatitis results in shorter hospital stays, less need for opioid painkillers, and fewer complications.
Compared with other surgical approaches, the laparoscopic form of total pancreatectomy with islet cell auto-transplantation may be an ideal option for some pancreatitis patients, surgeons report.
“In an era of opioid addiction, performing a major operation through a minimally invasive technique can mean less pain for patients, reducing the need for opioids and their complications,” says senior author Martin Makary, professor of surgery at Johns Hopkins University School of Medicine.
Every year, about 210,000 people in the United States are diagnosed with chronic inflammation of the pancreas, usually due to genetic mutations, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
Most of these patients experience long-term, difficult-to-manage pain. Placing a stent in the pancreas often fails, leaving patients the surgical option of removing the pancreas and “auto-transplanting” their own pancreatic islet cells into their liver. Those cells are needed to create insulin and control blood sugar.
Opioid use creeps back after weight-loss surgery
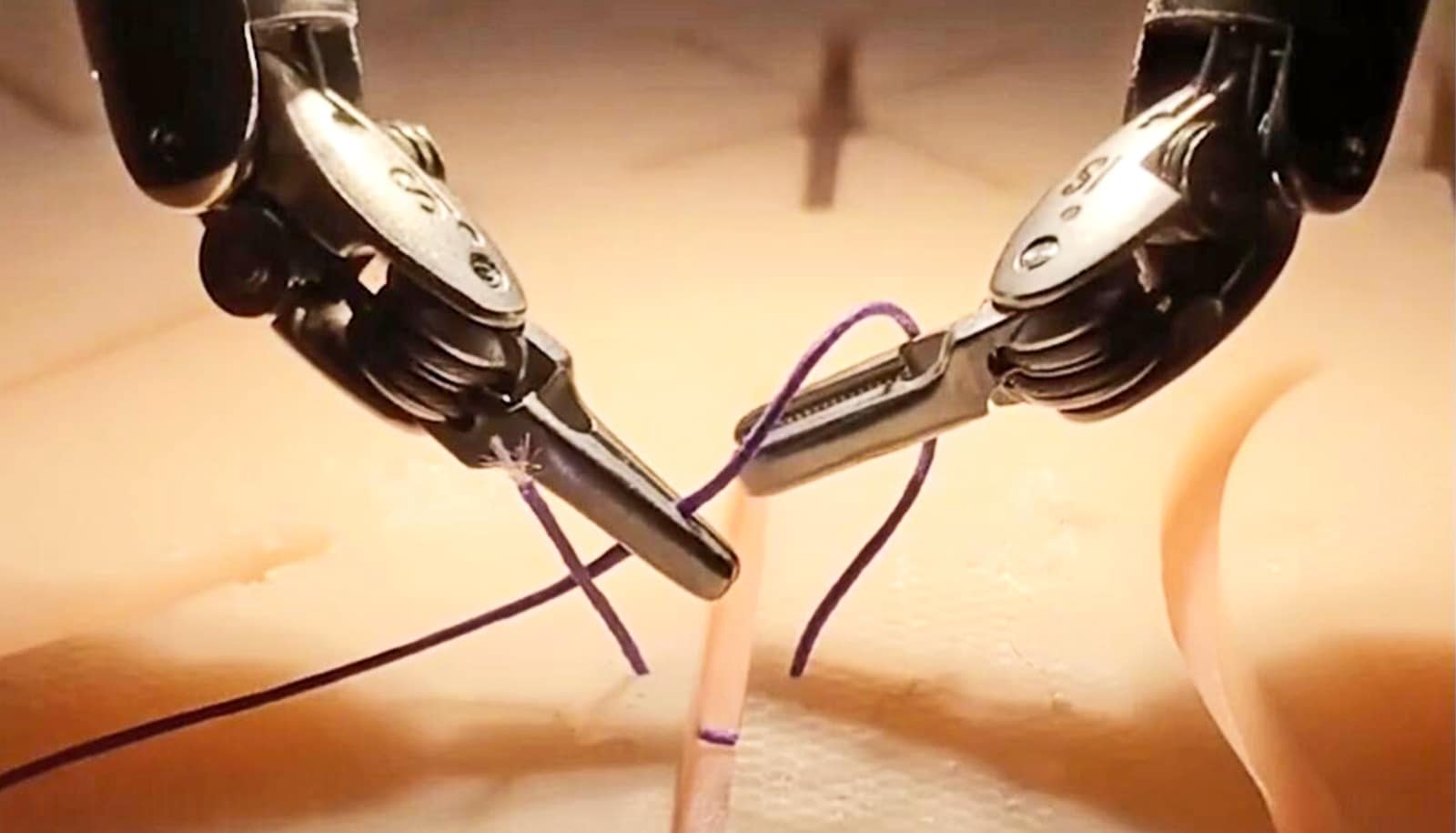
TPIAT is traditionally performed by opening a long incision in the abdomen to reach the pancreas and the liver. In recent years, less invasive operations have been developed. The latest involves the use of a laparoscope inserted into a small incision in the abdomen, through which a surgeon can manipulate instrument “hands” and small devices to perform the procedure.
Benefits of laparoscopic approaches can include vastly reduced risk of infection, a quicker recovery, and better pain management.
Makary and his team offered 20 Johns Hopkins Hospital patients with chronic pancreatitis the laparoscopic TPIAT operation from 2013 through 2015. Twelve of the 20 patients no longer required opioid therapy by their six-month follow-up.
Compared with other surgical approaches for TPIAT, this first series of laparoscopic TPIAT saw a shorter average operative time: an average of 493 minutes, versus 637.2, 533 and 712 minutes in studies of the older methods.
Average islet isolation time was 185 minutes, compared with more than 250, 240, 270 and 272.6 minutes. Length of hospital stay was 11 days, compared with 16, 12.6 and 12.6 days; patients also returned to work more quickly when operated on with the minimally invasive method.
“Chronic pancreatitis can be a very painful and debilitating condition,” Makary says. “Careful patient selection can match the right candidates to this new minimally invasive surgical therapy.”
The study appears in JAMA Surgery.
Source: Johns Hopkins University