The pathway in the body that leads to what laypeople call “hardening of the arteries” is not what medical experts previously assumed, report researchers who examined the mineralized arteries of genetically modified lab mice.
Mineralized arteries, a complication often seen in patients with chronic kidney disease and diabetes, may affect heart functions, leading to death in some instances.
Previously, McGill University team leader Marta Cerruti’s long-time collaborator Monzur Murshed and his trainees demonstrated that elastin, the material that gives arteries their elasticity so they can expand and contract in response to the pumping of the heart to facilitate blood flow, is a critical determinant of mineral deposition. Their study showed that collagen, which is essential for the normal mineralization of our bones and teeth, is not responsible for arterial mineralization.
“The first part that mineralizes in the arteries of our genetic model is the elastin part and not collagen,” says Cerruti, noting that this is very different from what happens in bone and teeth.
“To me, that was really surprising,” she says. “The part that mineralizes in bone and teeth is collagen. Since collagen is also present in the arteries, you would think collagen must have really specific properties that aid that process, so why do the minerals instead get deposited in association with elastin in arteries?”
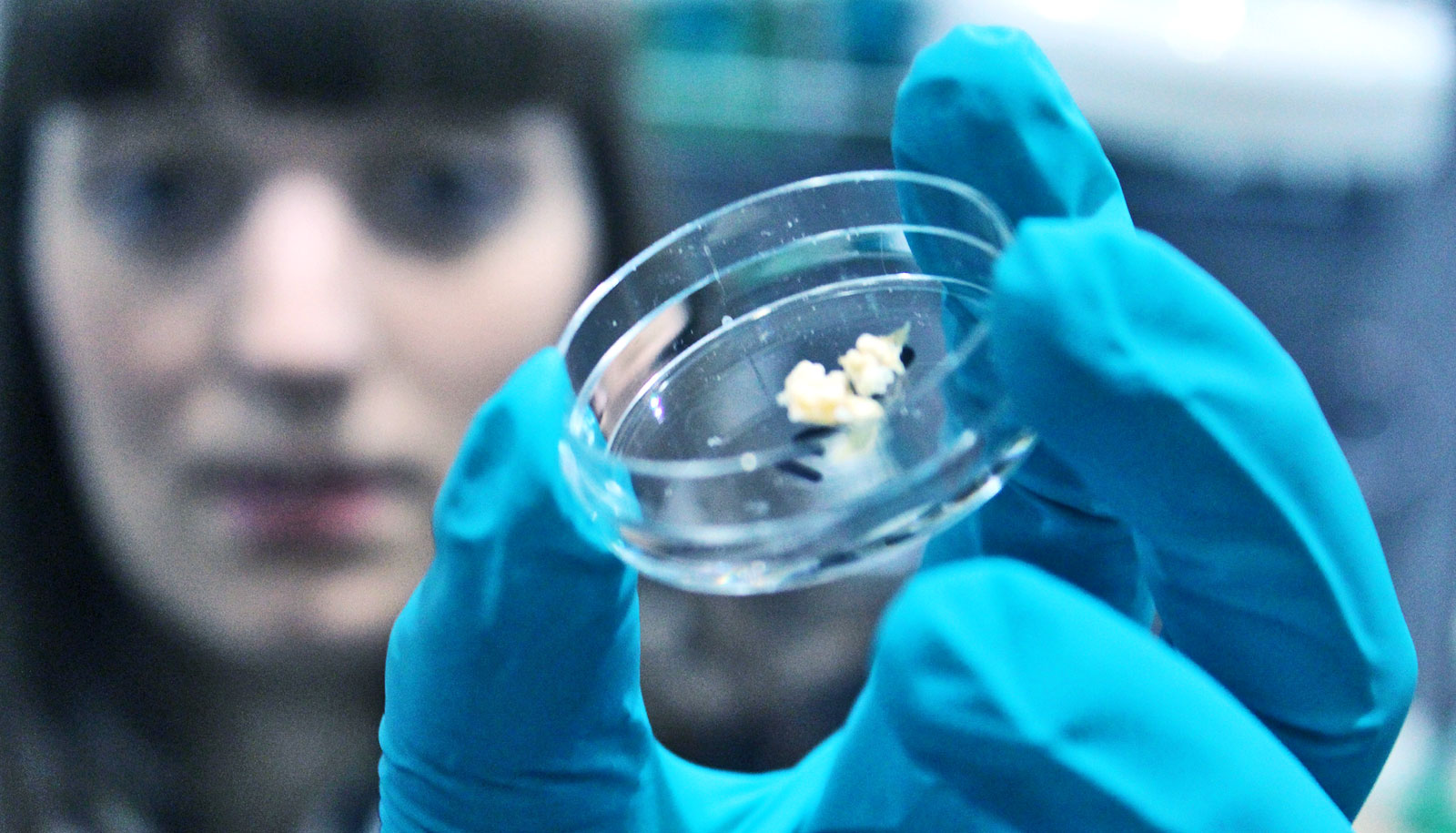
Using the Canadian Light Source’s SXRMB beamline, Cerruti’s team discovered the presence of early stage calcium phosphate minerals in the elastin-containing layers of the diseased mouse arteries.
Cerruti is hopeful the findings of this research will lead to a therapy that will block mineral accumulation in the arteries of patients who are prone to this condition.
People with unclogged arteries have more of this protein
The paper’s conclusion states that an effective strategy to prevent vascular calcification may involve intervening at the stage where calcium phosphate minerals begin crystallizing. It may be possible to selectively dissolve these nascent crystals with appropriately targeted drugs, the paper concludes.
Cerruti and Murshed, a coauthor of the new study, are leading a group to examine whether customized biomolecules can effectively block the process of mineral nucleation and/or crystal formation in the arteries at a very early stage.
As the research article explains, no current treatment for mineralization in arteries exists, largely because of lack of understanding of the underlying molecular mechanism. Cerruti expects her team will be back at the CLS as they work to refine their understanding of this stage of the mineralization process.
Cerruti expresses caution at this point and says her team’s paper only “hints” at a pathway forward to improving human health using a drug to treat a condition for which an effective treatment is still elusive.
Watch: Probe zooms through artery of living heart
“Maybe if we can stop the nucleation, we might be able to stop arterial mineralization,” she says.
The team’s latest study is published in the journal Arteriosclerosis, Thrombosis, and Vascular Biology.
Funding for the research came from a grant from the Heart and Stroke Foundation of Canada.
Source: McGill University